The Technology Assessment Unit - supporting optimal use of health technologies at the MUHC
 When a new piece of equipment comes on the market or a new drug boasts great benefits for our patients, our healthcare teams need a place to turn to help them decide whether or not to use them. The Health Technology Assessment Unit (TAU) of the MUHC was established precisely to respond to such challenges.
When a new piece of equipment comes on the market or a new drug boasts great benefits for our patients, our healthcare teams need a place to turn to help them decide whether or not to use them. The Health Technology Assessment Unit (TAU) of the MUHC was established precisely to respond to such challenges.
The TAU is an advisory group that supports clinical teams and the MUHC administration by providing an objective and transparent decision-making process to evaluate the overall value of new technologies and therapies using the best available scientific evidence.
A promising new cancer drug - plerixafor
Last year, the TAU was asked to look into a very promising drug, plerixafor. This new therapy is supposed to help stimulate the release of stem cells (stem cell mobilization), which is needed when treating patients with hematopoietic cancers, such as multiple myeloma and non-Hodgkin’s lymphoma.
These patients traditionally receive chemotherapy to stimulate the release of stem cells; however, chemotherapy has disadvantages, which include risk of hospitalization for side effects. Further, the unpredictability of chemo mobilization may prolong waiting times for stem cell transplants. The clinical team treating these patients was interested to know if plerixafor would work as well, or better than chemotherapy, particularly for reducing wait times for patients. On the other hand, there was the issue of cost – plerixafor is very expensive - – making it challenging to determine the preferred treatment approach.
TAU looked into three possible options for stem cell mobilization: i) upfront plerixafor, ii) pre-emptive plerixafor following chemotherapy; and iii) pre-emptive plerixafor following treatment with growth factors alone.
To read the full report click here.
The report concluded that a pre-emptive plerixafor regimen would be preferable to the use of upfront plerixafor due to the latter’s high cost impact. It highlighted that a pre-emptive regimen with growth factors alone would be the most attractive option. Treatment using growth factors alone had not been previously used at the MUHC since it is less effective in mobilizing stem cells compared with chemotherapy. However, use of growth factors in conjunction with plerixafor was determined to be the most attractive solution to the healthcare team and administration (Table).
The conclusion: by eliminating the use of chemotherapy for these patients shorter treatment times and wait times for stem cell mobilization can be ensured. This will increase hospital efficiency and access to care— a win-win solution for all.
For more information on the Technology Assessment Unit please contact Dr. Nandini Dendukuri, Director of the unit.
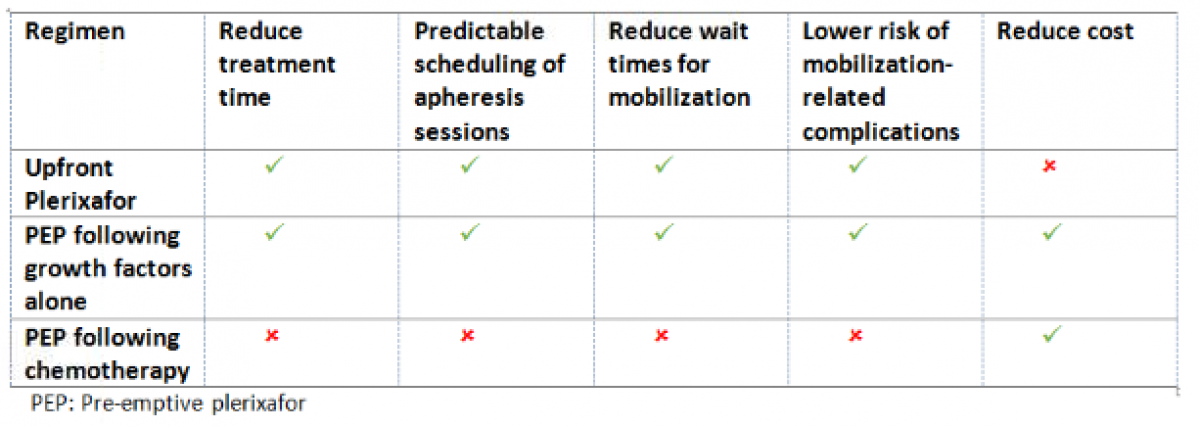
Table: Comparison of three stem cell mobilization regimens and their impact on patient- and hospital-important outcomes
