An organ chip that predicts the response to chemotherapy
With the development of a patient-specific organ-on-a-chip, Dr. Lorenzo Ferri at The Institute and collaborators at Harvard are advancing personalized cancer medicine.
Patients with advanced cancer who are still eligible for surgery typically receive neoadjuvant chemotherapy to shrink the tumour and improve surgical outcomes. However, some tumours are resistant to treatment—and clinicians currently have no way of knowing in advance which patients will benefit from chemotherapy.
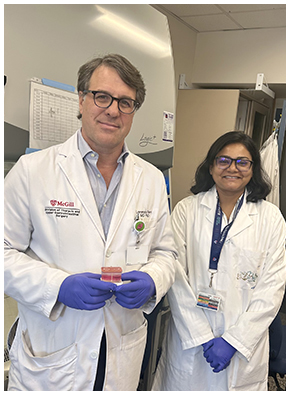
Thanks to a breakthrough in precision oncology led by Dr. Lorenzo Ferri at the Research Institute of the McGill University Health Centre (The Institute) and Dr. Donald Ingber at the Wyss Institute for Biologically Inspired Engineering at Harvard University, this reality could soon change. Together, they have developed a small device called an organ-on-a-chip, or organ chip, which recreates a patient’s cancer and surrounding tissues to predict how it will respond to treatment. This technology could help physicians avoid giving patients therapies unlikely to work for them, and instead guide them toward options with a greater chance of success.
“This is the first time we have been able to reproduce, outside the body, not only a person’s cancer but also the surrounding support cells and proteins—in a way that predicts treatment response very precisely,” says Dr. Ferri, Director of the Division of Thoracic and Upper Gastrointestinal Surgery at the McGill University Health Centre (MUHC) and Senior Scientist in the Cancer Research Program at The Institute. “This innovation has the potential to directly improve patient outcomes by enabling clinicians to match each patient with the therapies best suited to them.”
Accurate predictions in the clinic
As part of this work, recently published in the Journal of Translational Medicine, researchers developed a personalized organ chip for eight patients treated at the MUHC for esophageal adenocarcinoma, a cancer with a very high mortality rate. Each organ chip was exposed to the same chemotherapy protocol as the patient, at the same time and at the same dose.
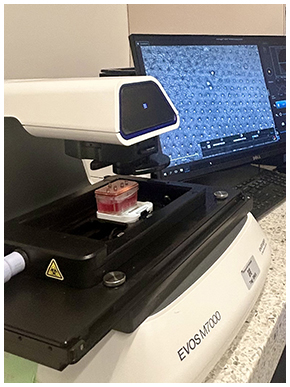
In the cohort of eight patients, all of the chips accurately predicted the response to neoadjuvant chemotherapy in just 12 days. In four chips, the treatment caused cancer cell death, while in the other four, the cells survived. These results matched perfectly with the patients’ actual responses to the same chemotherapy, as well as with their survival rates following surgical removal of the tumour.
“The perfect match between chip results and patient outcomes suggests that the model could become a powerful tool to support decision-making in clinical practice,” adds Dr. Ferri, who is also the David S. Mulder Chair of Surgery at McGill University.
Recreating the tumour and its surrounding microenvironment
The organ-on-a-chip developed in the study builds on two existing technologies: organoids and microfluidic organs-on-chips.
Organoids—tiny mini organs made up of clusters of cells grown from a patient’s tumour—can mimic many characteristics of cancerous tissue. The study’s first author, Sanjima Pal, PhD, along with other members of Dr. Ferri’s team, have developed remarkable expertise in creating patient-specific esophageal organoids with great consistency.
“However, to determine how a cancer responds to treatment, these organoids lack important elements of the tumour’s microenvironment, such as stromal cells and the connective tissues surrounding the tumour,” explains Pal, Scientific Research Manager in Dr. Ferri’s team. “To address these gaps and better capture the complexity of the tumour, we drew on the human organ-on-a-chip microfluidic culture technology developed at the Wyss Institute.”
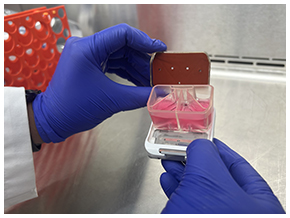
The team first created organoids from biopsies taken by endoscopy from newly diagnosed patients who had not yet received treatment. They then transferred and cultured cells from these organoids into one of the channels of a small microfluidic chip, about the size of a memory stick, and placed stromal fibroblasts from the same tumour into a parallel channel to recreate the actual tumour environment. On the chip, the two channels are separated by a porous membrane that enables the cancer and stromal cells to exchange molecules, just as they would inside the body.
Finally, the team circulated through the chip the chemotherapy drugs used in the clinic, replicating the same concentrations and exposure times as in the actual treatment given to the patient.
“Not only was the organ chip able to recreate the microscopic appearance and DNA of the patient’s tumour, but it also reproduced the response to chemotherapy more accurately than organoids had in previous studies,” adds Dr. Ferri.
Unlocking potential to bring precision oncology to patients
This technology paves the way for major advances, as it could:
- Personalize treatments for resistant cancers by testing each patient’s tumour to assess its sensitivity to standard chemotherapy and, if needed, explore other therapeutic options.
- Develop and validate new targeted therapies for different cancers.
- Identify biomarkers to monitor and optimize the effects of drugs in patients.
Dr. Ferri hopes to launch a clinical trial within the next year to bring the most promising cancer treatments to patients while sparing them the side effects of ineffective options. With his team, he is also working to adapt the chip for other types of tumours where chemotherapy is widely used but not always effective, including stomach cancer, lung cancer, and mesothelioma.
“Being able to predict whether a chemotherapy regimen will work for a given patient could be transformative,” says Dr. Ferri. “Even more importantly, this innovation opens up exciting new possibilities for drug discovery and precision oncology — not only for gastrointestinal cancers, but for many other types of cancer as well.”
About the study
Patient-derived esophageal adenocarcinoma organ chip: a physiologically relevant platform for functional precision oncology, by Sanjima Pal, Elee Shimshoni, Salvador Flores Torres, Mingyang Kong, Kulsum Tai, Veena Sangwan, Nicholas Bertos, Swneke Donovan Bailey, Julie Bérubé, Donald E. Ingber and Lorenzo Ferri was published in the Journal of Translational Medicine.
DOI: https://doi.org/10.1186/s12967-025-06593-1
This study was funded by the Montreal General Hospital Foundation with the invaluable support of the Jarislowsky Foundation, as well as the United States Department of Defense and Cancer Research UK Grand Challenge.
The researchers thank the study participants for generously allowing the use of their biological samples and clinical data, as well as the MUHC pathology service for determining tumour content in primary tissues, and Génome Québec for its role in acquiring whole-exome sequencing data. In addition, they are grateful to the biobank and the histopathology and molecular imaging platforms at the Research Institute of the McGill University Health Centre (The Institute), as well as the histology platform at McGill University’s Goodman Cancer Institute, for their support.
Media contact
Fabienne Landry
Communications coordinator, Research, MUHC
[email protected]
