Less movement, less spread of infection
In collaboration with the emergency department’s leadership team, Natasha Dupuis, an advanced practice nurse clinician in the emergency department of the McGill University Health Centre (MUHC), is deploying tools to limit patient movement in the emergency department. In 2020, in the midst of the pandemic, she successfully implemented a state-of-the-art technological system for the emergency department.
“At the beginning of the pandemic, our team was trying to identify ways to reduce the movement of patients in our institution, and at the same time, the risk of spreading infections, says Natasha Dupuis. We were also looking for ways to reduce the time between a request for an electrophysiology consultation and the results of the exam. So we decided to look at the CareLink Express Mobile application.”
This application helps to remotely manage implanted cardiac devices (pacemakers) from any patient care setting in the hospital, i.e., intensive care, in-house consultation, catheterization laboratory, surgery centre and patient clinic, in order to quickly perform device checks and receive a remote technical assessment of its status.
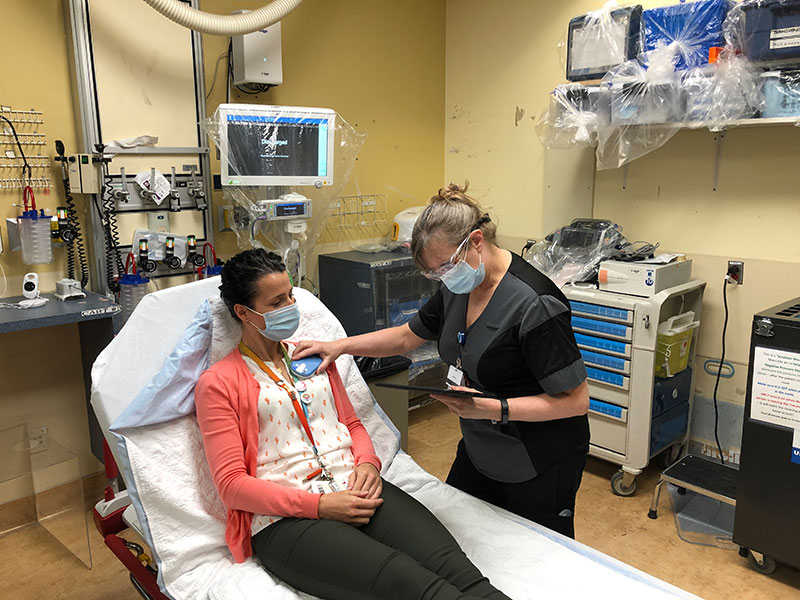
“The only equipment needed is a tablet and a patient connector. The electrophysiology and emergency teams worked together to develop a care protocol to guide the treating teams in using the new technology. Once we were ready, we deployed with the teams,” says Natasha.
The system has proven to be easy to use: the application on the tablet is straightforward, intuitive, and even a first-time user can find his way around easily. The patient connector has only one button to turn it on or off, and an indicator light shows whether it is connected to the pacemaker. “We trained the majority of the clinical team, and even those who had not received training were able to use the device easily. I’ve seen clinicians who were apprehensive about the new technology—and have admitted that it’s quite simple to use,” says Natasha.
Basically, the emergency doctor determines whether a pacemaker interrogation is necessary and then communicates this information to the nurse. The nurse then gets the tablet and the patient connector and goes to the patient’s bedside. The nurse can then perform the interrogation and notify the administrative officer that the interrogation has been completed so that she can call the electrophysiology team.
This system has many advantages. “Considering the current situation, reducing the risk of spreading infections is certainly an interesting aspect because trajectories are optimized and patient wait times are reduced. In addition, considering our responsibility for access, quality of care, and the patient experience, remote services become an interesting option in the development of our programs. For example, Medtronic’s CareLink Express Mobile system could be deployed in remote facilities such as Northern Quebec, making patient investigations possible without having to bring them to Montreal.”
