National Pain Awareness Week: evaluating, documenting and treating
A visit to an emergency department can be a trying time for anyone, but for elderly patients experiencing pain, attempting to put symptoms into words takes “trying” to a whole new level.

Dr. Suzanne Morin, Marie-Andrée Jacques and Valérie Bassien-Capsa
This is the main motivator behind the PAINFREE initiative at the McGill University Health Centre (MUHC). With tools and training, emergency department (ED) staff are now armed and able to better support this patient population, who come in with pain.
The initiative was launched when the MUHC granted the project $150,000 through the 2012 Challenge Q+ award—an MUHC quality improvement strategy built to encourage innovation and creativity in patient care. The leader of this initiative is Dr. Suzanne Morin, Clinician Scientist of the MUHC Division of General Internal Medicine. It’s a massive team effort, and has been developed in collaboration with emergency room physicians, nurses, and pharmacists.
“The goal of the PAINFREE project, which stands for Improving PAIN control following FRactures; towards an Elder-friendly Emergency department, is to improve acute pain management for older adults, including those with cognitive impairment, who arrive in the ED with a low-trauma bone fracture,” Dr. Morin explains.
Moving forward, making progress
A lot has happened since 2012, including a pilot phase following the Challenge Q+ Award. It was a chance for the team to develop their tools, their message, and their plan of action by speaking with patients, doctors, and nurses—with the ultimate goal of designing a better plan for intervention.
Thanks to the success of the pilot study, Dr. Morin and her team were able to receive a Canadian Institute of Health Research grant with a plan to have the program implemented in six different emergency departments across the Island of Montreal. The six institutions that have currently signed onto the project are the MUHC, St. Mary’s Hospital, The Jewish General Hospital, The Lakeshore General Hospital, Hôpital de Verdun, and Hôpital Sacré-Coeur.
“We are implementing the project in a sequential fashion, two institutions at a time. It's a multifaceted intervention whereby we focus our interventions on nurses, the physicians, the patients, and the environment,” says Dr. Morin.
The two institutions currently running the project are the MUHC emergency departments at the Montreal General Hospital and Royal Victoria Hospital, and St. Mary’s Hospital.
The process
Every health care professional working on the specific sites is encouraged to attend an accredited educational session in order to become familiar with the tools developed to better assess, document, and treat pain in the ED.
It’s important not to forget the patients and their families. Once they have been discharged, the project ensures that they are equipped to handle the pain upon their return home. Educational resources developed in collaboration with the MUHC Patient Education Office to empower patients, such as a bilingual information booklet, are also available online.
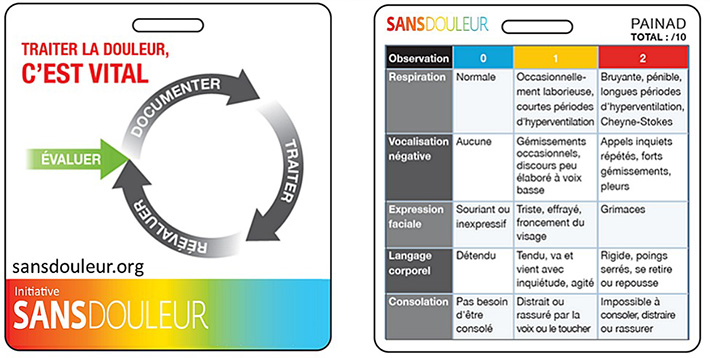
The PAINAD card is worn by nurses in the emergency departments, allowing them to assess the pain score for patients. Observations are made based on breathing, negative vocalization, facial expression, body language, and consolability of the patient.
Patient resources = patient autonomy
As Dr. Morin explains, pain that goes untreated can lead to agitation, confusion, and extreme discomfort. There are also knowledge gaps surrounding medications used to treat pain. Information surrounding medication is made accessible to patients through the program.
“There is a lot of information in the booklet on medication, and on how to act at home in order to be comfortable,” says Valérie Bassien-Capsa, research coordinator at the Research Institute (RI)-MUHC and PAINFREE project coordinator. “Once a patient returns home they don’t always know what to do, so these are good companion tools for patients and their families.”
The project, while in the beginning stages, is showing positive results across the board. Nurses are better equipped to treat pain, and as a result will likely be more efficient.
“For the patients, the intervention is quicker, and therefore the return home is quicker. The faster their pain is managed, the less they experience side effects. That means the faster they can be mobile again,” says Marie-Andrée Jacques, an MUHC nurse educator who is part of the PAINFREE team.
What’s next?
In order to assess the effectiveness of the project, Dr. Morin and her team will be collecting information on indicators of pain management. In the meantime, planning is underway in order to implement the project at Hôpital de Verdun and Hôpital Sacré-Coeur.
“We are very happy that this project is moving forward, and we hope to have a positive impact on quality care for elderly patients,” says Dr. Morin.
