Honouring the powerful legacy of Dr. Balfour M. Mount, 1939-2025, the father of palliative care in Canada
 It seems that lately we are having to say goodbye too frequently to healthcare professionals who have shaped our practices and curricula, as well as the critical work of those who have followed in their footsteps. Today, I share the sad news that Dr. Balfour M. Mount passed away on September 25, 2025, at the age of 86, in the palliative care unit bearing his name at the Royal Victoria Hospital (RVH) of the McGill University Health Centre (MUHC). I also wish to reflect on Dr. Mount’s journey towards being recognized as the father of palliative care in Canada through the lens of excellence and innovation, pillars which I espouse as essential to transforming our patients’ experience and outcomes.
It seems that lately we are having to say goodbye too frequently to healthcare professionals who have shaped our practices and curricula, as well as the critical work of those who have followed in their footsteps. Today, I share the sad news that Dr. Balfour M. Mount passed away on September 25, 2025, at the age of 86, in the palliative care unit bearing his name at the Royal Victoria Hospital (RVH) of the McGill University Health Centre (MUHC). I also wish to reflect on Dr. Mount’s journey towards being recognized as the father of palliative care in Canada through the lens of excellence and innovation, pillars which I espouse as essential to transforming our patients’ experience and outcomes.
In 1973, Dr. Mount was a practicing urologist and surgical oncologist at the RVH when he conducted a study of the care provided to terminally ill patients and their families. The study revealed that patients reaching the end of their lives received inadequate care across all services, often leading to unintentional neglect, distress and isolation. His desire to change the situation led him to join internationally-renowned end-of-life pioneer Dr. Cecily Saunders and her team at St. Christopher’s Hospice in London, England, as a visiting professor, having heard about her hospice-care model through Elisabeth Kübler-Ross’ book On Death and Dying. Upon his return to Montreal in 1974, he transplanted what he had learnt and adapted it to Quebec’s reality for the benefit of our patients and their family members.
 Assuring that people lived without discomfort at the end of their life was of paramount importance to Dr. Mount when he established North America’s first Palliative Care Service (PCS) at the RVH. Moreover, it was vital to him that the quality of care not be subjugated by budget restrictions and other demands on the healthcare system. Indeed, the hospital took a leap of faith when the service was launched because it was juggling both budget and bed shortages. As a result of his courage and the support of hospital leadership, Dr. Mount delivered a model of excellence that was ahead of its time, which included a home care program, inpatient ward, consultation service, bereavement follow-up team, as well as research and teaching. He associated the service with the word palliative because its etymology is to improve the quality of and this resonated with him. The PCS team went on to publish The RVH Manual on Palliative/Hospice Care, a volume that became the reference text for developing palliative care services across the country and broadened the traditional concept of physical health care to include the psychosocial, spiritual and existential challenges of advanced disease.
Assuring that people lived without discomfort at the end of their life was of paramount importance to Dr. Mount when he established North America’s first Palliative Care Service (PCS) at the RVH. Moreover, it was vital to him that the quality of care not be subjugated by budget restrictions and other demands on the healthcare system. Indeed, the hospital took a leap of faith when the service was launched because it was juggling both budget and bed shortages. As a result of his courage and the support of hospital leadership, Dr. Mount delivered a model of excellence that was ahead of its time, which included a home care program, inpatient ward, consultation service, bereavement follow-up team, as well as research and teaching. He associated the service with the word palliative because its etymology is to improve the quality of and this resonated with him. The PCS team went on to publish The RVH Manual on Palliative/Hospice Care, a volume that became the reference text for developing palliative care services across the country and broadened the traditional concept of physical health care to include the psychosocial, spiritual and existential challenges of advanced disease.
End-of-life care policies, practices and laws may have evolved in the years since Dr. Mount practiced and taught, but improving the quality of patients’ experience and outcomes is as central to our teams’ thinking as it was to that of his team. When the concept of medical aid in dying legislation was being introduced, for example, Dr. Mount thought investments in end-of-life care to alleviate suffering should be prioritized instead. However, I believe the principles of improving the quality of care and dying without discomfort today echo the spirit if not the letter of his holistic vision and values. After all, knowledge begets new knowledge. We model the future we want for our patients by listening, learning, collaborating and balancing next-generation technology and equipment with supportive and palliative care that addresses the whole-person-care needs of those in all stages of illness at the end of their life.
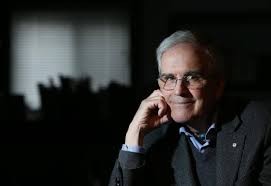
Dr. Balfour M. Mount was a caring physician, skilled surgeon, founding director of the Royal Victoria Hospital Palliative Care Service of the MUHC, Eric M. Flanders Emeritus Professor of Palliative Medicine, founding director of the Palliative Care Division in the Department of oncology and creator of the McGill Programs in Whole Person Care at McGill University. An enthusiastic teacher who received McGill’s Osler Teaching Award, Dr. Mount also initiated McGill’s biennial International Congresses in Care of the Dying. He authored over 150 publications, including Sightings in the Valley of the Shadow: Reflections on Dying and his memoir Ten Thousand Crossroads: The Path as I Remember It, participated in teaching films and audiotapes, and was a guest lecturer and professor in Canada and the United States, as well as in Europe and on other continents around the globe.
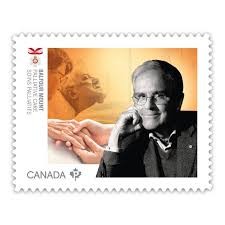 In Dr. Mount’s lifetime, various organizations recognized his exceptional contributions to palliative care, not least of which the MUHC when it rightfully named The Balfour Mount Palliative Care Unit, a 12-room unit offering holistic care through an interdisciplinary team of nurses, physicians, psychologists, a social worker, music therapist, spiritual care worker and a host of other allied health professionals. Dr. Mount was inducted into the Canadian Medical Hall of Fame, conferred the title of Officer by the Order of Canada and Ordre national du Québec and made a member of the Academy of Great Montrealers. A recipient of the Canadian Palliative Care Association’s Award of Excellence and American Academy of Hospice and Palliative Medicine’s Lifetime Achievement Award, Canada Post also commemorated him with a Medical Groundbreaker stamp.
In Dr. Mount’s lifetime, various organizations recognized his exceptional contributions to palliative care, not least of which the MUHC when it rightfully named The Balfour Mount Palliative Care Unit, a 12-room unit offering holistic care through an interdisciplinary team of nurses, physicians, psychologists, a social worker, music therapist, spiritual care worker and a host of other allied health professionals. Dr. Mount was inducted into the Canadian Medical Hall of Fame, conferred the title of Officer by the Order of Canada and Ordre national du Québec and made a member of the Academy of Great Montrealers. A recipient of the Canadian Palliative Care Association’s Award of Excellence and American Academy of Hospice and Palliative Medicine’s Lifetime Achievement Award, Canada Post also commemorated him with a Medical Groundbreaker stamp.
Such recognition is a testament to his legacy, but I would like everyone to consider that his gift to us—much like that of other MUHC-McGill luminaries—is to continue to inspire excellence and the individual and collective courage to tackle with tenacity of purpose, humility and compassion the healthcare issues of our day so that we always innovate for our patients and their families.
Lucie Opatrny, MD MSc MHCM FRCPC
President and Executive Director – MUHC
