
Hypertrophic Cardiomyopathy
What is hypertrophic cardiomyopathy, and how does it affect the heart?
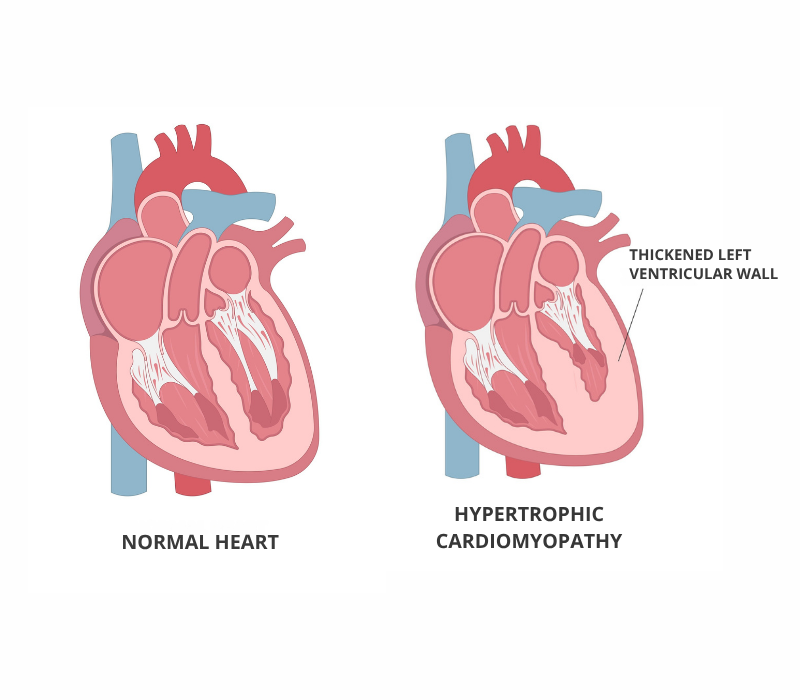
Hypertrophic cardiomyopathy (HCM) is a condition that impacts the heart muscle (called the myocardium), particularly the left ventricle. In HCM, the heart muscle becomes thicker (called hypertrophied), which can make the heart muscle stiff and make it harder for the heart to pump blood effectively. This thickening can lead to narrowing of the heart’s chambers, obstructing blood flow. In some people, HCM can lead to serious complications, including arrhythmias, heart failure and sudden cardiac arrest.
HCM is the most common inherited heart disease. It can affect people of all ages. HCM affects both men and women. It is estimated to affect one in every 500 people.
Many people with HCM may never experience any symptoms, but the condition most often shows up in people between the ages of 20 and 60. Sometimes it is diagnosed during childhood or in adults over the age of 60.
Many people with HCM have no symptoms or very mild symptoms.
The most common symptoms include:
- shortness of breath (especially with exercise)
- palpitations (heartbeats that feel strange)
- chest pain
- dizziness/lightheadedness
- syncope (fainting caused by a cardiovascular issue), especially with exercise.
- fatigue
- sudden cardiac arrest (in severe cases)
It is important to note that experts may not be able to identify a cause of HCM in some patients (even those with a family history of HCM).
The most common causes of HCM are:
- genetics (familial cases or those with a genetic change related to HCM)
- underlying health conditions (rare)
- secondary thickening due to long-term high blood pressure
A genetic cause can be found in approximately 30 per cent of patients with HCM. There can also be more than one cause, for example a combination of a genetic and lifestyle factors.
- medical and family history
- angiogram
- blood tests
- echocardiogram
- electrocardiogram (ECG/EKG)
- cardiac MRI (Magnetic Resonance Imaging)
- genetic testing
- exercise stress test
- chest x-rays
There is no cure for HCM, but there are treatments available to manage symptoms and reduce the risk of complications. Treatment may vary depending on the severity of the condition and the patient's needs. It may include:
- medications (beta-blockers, calcium channel blockers, antiarrhythmic drugs, etc.)
- lifestyle changes, such as limiting alcohol intake and drug use, eating heart-healthy foods (lean proteins, vegetables and fruits and low-salt food) and increasing physical activity
- minimally invasive procedures, such as implanting a pacemaker or an implantable cardioverter defibrillator (ICD)
- surgical procedures, such as septal myectomy (removal of part of the thickened muscle) or ablation
- heart transplant (in very severe cases in which other treatments have failed)
HCM is primarily hereditary, so prevention focuses on early detection and management.
If you or a family member has been diagnosed with HCM, it’s important to monitor heart health regularly and take steps to reduce risk factors within your control. This includes:
- avoiding recreational drugs, such as cocaine
- keeping alcohol intake to a moderate level
- managing any health condition that could increase your risk of HCM, such as diabetes and high blood pressure
- choosing to live a healthy lifestyle, such as eating healthy foods and exercising daily
- going for regular cardiovascular check-ups
I am a patient diagnosed with HCM. What do my genetic test results mean?
A negative genetic test means that no mutations associated with HCM were identified in your DNA. However, it’s important to remember that not all genetic mutations causing HCM are known or detectable at this time.
Approximately 30 per cent of individuals with HCM will have a positive genetic test. A negative test result doesn’t rule out a genetic predisposition entirely. We recommend that your immediate family members (parents, siblings, and children) undergo regular check-ups every three to five years to ensure early detection.
Remember: a negative genetic test result doesn't change your diagnosis or affect the care plan that you have with your cardiologist.
A positive genetic test result means that a genetic change (also called a variant) responsible for HCM has been identified in your DNA. This confirms the genetic nature of your condition, but it doesn’t help us know how the condition will develop or which symptoms you may develop. Some people with the mutation may remain asymptomatic throughout their lives, while others may develop symptoms of HCM.
Sometimes when a mutation is identified we may consider the possibility of implanting an ICD. This may be discussed during your follow-ups with HCM experts.
Some mutations may also be found in genes related to symptoms affecting other organs in your body. If this is the case, you will discuss this with a genetic expert.
In most cases, the risk of transmitting the mutation to your children is 50 per cent, or 1 in 2. Your parents and siblings also have 50 per cent risk of having this mutation.
A variant of uncertain significance (VUS) means that a genetic variation was found, but there isn’t enough scientific evidence to confirm whether it causes HCM.
When such a result is identified, we consider it as inconclusive and do not recommend testing this variant in family members. This result is usually treated like a negative result and we recommend clinical evaluations for immediate family members. If a family member has the same symptoms as you, we may consider testing the variant and evaluating its impact in the family.
You and your family are asked to stay in contact with the clinic and reach out in two to three after these test results to revise any necessary information.
I am a family member of a patient diagnosed with HCM. What should I expect?
You've been found to have the same mutation as a family member diagnosed with HCM, but you don't have any symptoms. This is common in cardio-genetics. Genetic conditions like HCM are complex, and other factors such as age and lifestyle may influence whether or not symptoms appear.
Having the mutation doesn't mean you will develop symptoms of HCM. Symptoms can vary among family members who carry the same mutation. Your cardiologist will likely ask for yearly check-ups to monitor your heart health and catch any issues early.
You are not at an increased risk of developing the condition. You do not need specialized screenings for HCM, and you will not pass the mutation on to your children. However, maintaining a healthy lifestyle and getting regular check-ups is still important to protect your overall cardiovascular health.
