
Dilated cardiomyopathy
What is dilated cardiomyopathy, and how does it affect the heart?
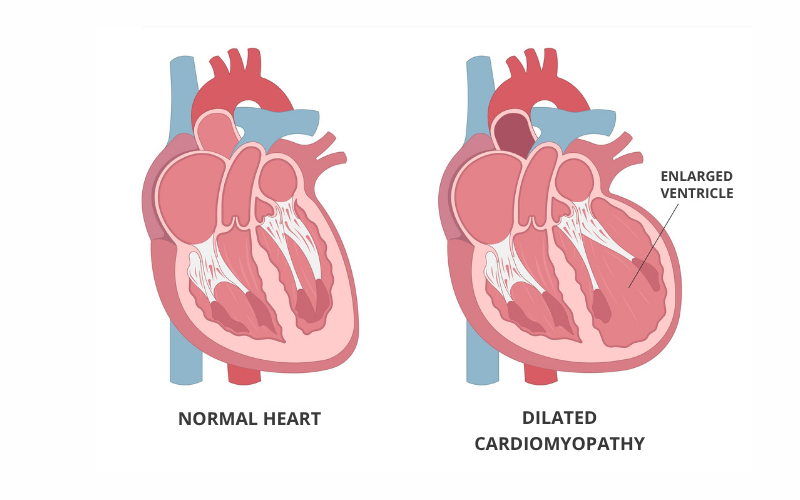
Dilated cardiomyopathy (DCM) is a condition that affects the heart muscle, especially the left ventricle. In DCM, the heart muscle becomes thinner and weaker, making it harder for the heart to pump blood through the body. As the muscle weakens, the left ventricle can stretch and enlarge, which is where the term 'dilated' comes from. If not treated in time, the heart struggles to pump blood properly, causing fluid to build up in the body. This can lead to heart failure.
DCM is more common in men than in women, but anyone can be affected. It is estimated that DCM affects 36 patients in every 100,000. Symptoms usually start between the ages of 20 and 60.
- chest pain
- dizziness/lightheadedness
- syncope (fainting that is caused by a cardiovascular issue)
- fatigue
- palpitations (heartbeats that feel strange)
- shortness of breath
- swelling in the legs and feet
Sometimes a cause cannot be identified, but the most common causes are:
- abnormal heart rhythms (arrhythmias)
- alcohol and/or drug abuse
- certain types of chemotherapy
- hormonal changes (especially during pregnancy)
- congenital heart disease
- diabetes
- genetics
- heart attack
- heart valve disease
- high blood pressure
- myocarditis
- infectious diseases (for example, HIV or viral hepatitis)
- thyroid disease
In about 29 per cent of patients with DCM, there is a genetic cause. There can also be more than one cause, for example a combination of genetic and lifestyle factors.
- medical and family history
- angiogram
- blood tests
- echocardiogram
- electrocardiogram (ECG/EKG)
- exercise stress test
- genetic testing
- cardiac magnetic resonance imaging (MRI)
- chest x-Rays
- muscular biopsy (rare)
DCM cannot be cured, but it can be managed. Treatment plans vary and may include:
- medications
- lifestyle changes, such as limiting alcohol intake and drug use, eating heart-healthy foods (lean proteins, vegetables and fruits and low-salt food) and increasing physical activity
- minimally invasive procedures, for example implanting a pacemaker or an implantable cardioverter defibrillator (ICD)surgery, for example ablation
- heart transplant
If you or a member of your family has tested positive for a mutation associated with an increased risk of developing DCM, it’s important to take steps such as:
- avoiding recreational drugs such as cocaine
- keeping alcohol intake to a moderate level
- managing health conditions that could increase your risk of DCM, such as diabetes and high blood pressure
- eating healthy foods and exercising daily
I am a patient diagnosed with DCM. What do my genetic test results mean?
This result is inconclusive. Even though your test result is negative, we recommend that your immediate family members (parents, siblings, and children) have regular check-ups with their doctor every three to five years. These check-ups should include an echocardiogram and electrocardiogram.
Remember: the negative genetic test result doesn't change your diagnosis or affect the care plan that you have with your cardiologist.
If a mutation is identified in a gene associated with DCM, it confirms the genetic nature of the condition. This result doesn’t tell us how the condition may develop or which type of symptoms you may experience.
Sometimes when a mutation is identified, we consider the possibility of implanting an ICD. If this is an option in your case, it may be discussed during your follow-ups with the DCM experts.
Some mutations may also be found in genes related to symptoms affecting other organs in your body. If this is the case, this will be discussed with you by a genetic expert.
In most cases, the risk of transmitting the mutation to your children is 50 per cent or 1 in 2. Your parents and siblings also have a 50 per cent risk of having this mutation.
Sometimes a variation in genes known to be associated with DCM may be found, but the scientific information on this variant is limited. These variants are called variants of uncertain significance (VUS).
This type of result is inconclusive and we do not recommend testing this variant in family members. This is treated like a negative result, and clinical evaluations for close family members are recommended. If a family member has the same symptoms as you, we may consider testing for the variant and evaluating its impact in the family.
You and your family should be re-evaluated in two to three years.
I am a family member of a patient with DCM. What should I expect?
You have the same mutation as a family member who is diagnosed with DCM, but you don't have any symptoms. This is common in cardio-genetics. DCM is a complex condition that can be influenced by small genetic changes and environmental factors.
Having the mutation doesn't mean you will develop symptoms of DCM. Your cardiologist will likely ask for yearly check-ups to monitor your heart health so, if any issues develop, they are caught early and can be treated. If you have children, they have a 50 per cent risk of inheriting the same mutation. Genetic screening will be available to them.
You’re not at an increased risk of developing DCM. There’s no need for specialized screenings for DCM. You didn’t inherit the mutation, so you can’t pass it on to your children.
