A chance at fatherhood after testicle cancer
Greg Star was 22 years old when he suspected he had a tumour in his testicle.
“I had a terrific pediatrician who taught me how to do the self-examination,” he says. “In February 2004, I noticed a mild discomfort in my left testicle, so I checked it and realized something was not quite right.”
After some tests, Star was diagnosed at the at the Royal Victoria Hospital of the McGill University Health Centre (RVH-MUHC) with testicular cancer, the most common form of cancer in men between the ages of 15 and 34. He had surgery that very same day.

“It was scary. They wanted to remove it as quickly as possible to prevent the cancer from spreading. There was a month of recovery and then chemotherapy began.”
A week after surgery, one of Star’s urologists, Dr. Peter Chan, suggested he bank his sperm.
“Dr. Chan told me ‘You’re probably not thinking about it right now, but you’re likely going to want to store some sperm, because chemotherapy can affect your fertility down the road.’ I had other plans for my life at the time, but I did some research and decided I would definitely regret not doing it. So I made an appointment at the MUHC Reproductive Centre to have some of my sperm frozen.”
“As soon as they call us, cancer patients can give one, two, three samples that can be frozen before they start cancer therapies. We give them a chance to have a biological child should they become sterile.” – Dr. William Buckett, medical director, MUHC Reproductive Centre.
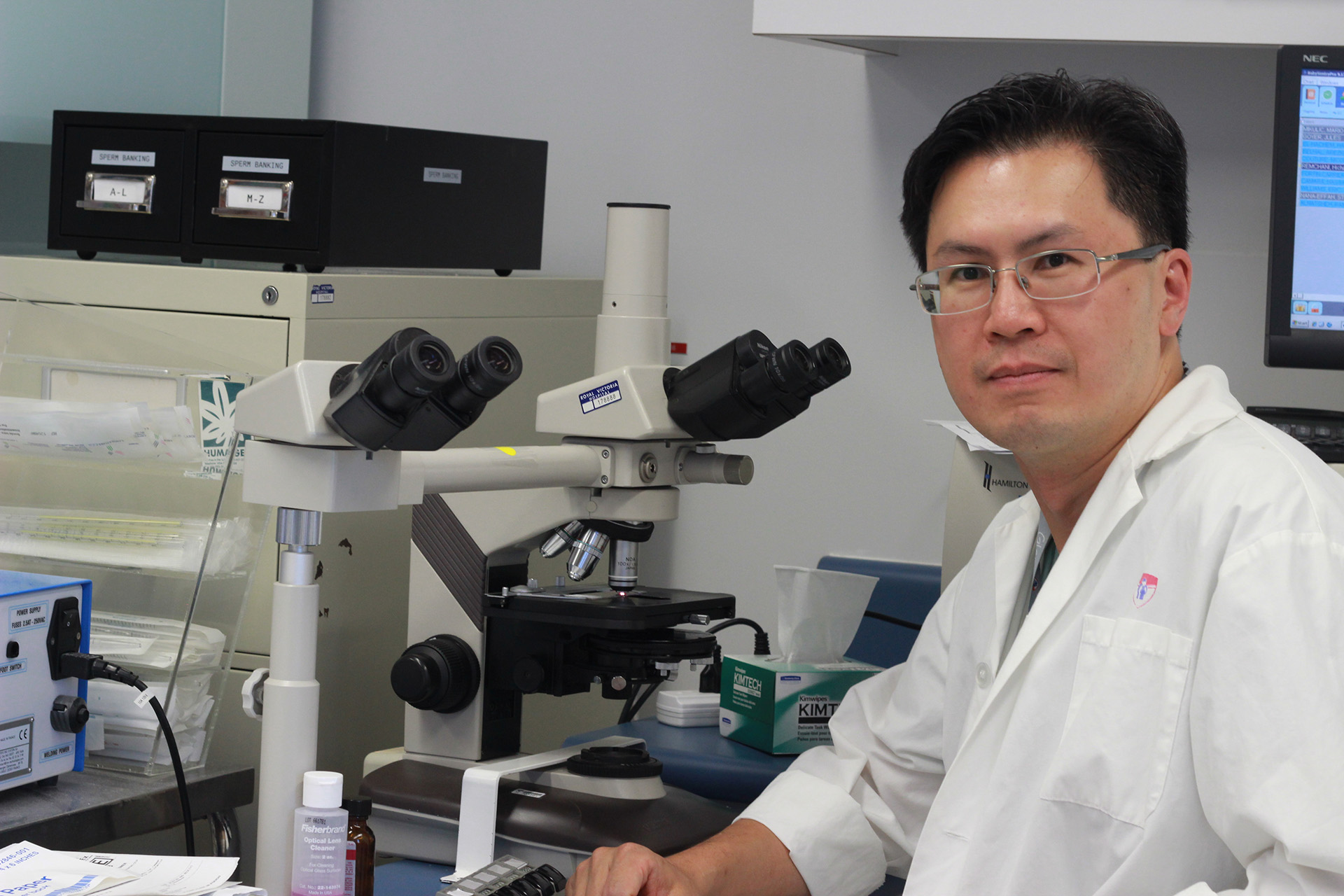
“Sperm cryopreservation or sperm banking is very important,” says Dr. Chan, who is also director of Male Reproductive Medicine at the MUHC and associate professor of Surgery at McGill University. “Even though the treatment for testicular cancer is highly effective – the survival rate is more than 90 per cent over five years – surgery, chemotherapy or radiation can have serious and lasting effects on the reproductive organs and on fertility.”
One of Dr. Chan’s goals is to create more awareness within oncology and psycho-social services, and the Reproductive Centre to better inform MUHC cancer patients about sperm cryopreservation.
“These young men are fighting cancer. They are not thinking about their fertility or about starting a family,” says Dr. Chan. “But they might in the future. So oncologists could definitely improve the quality of life of cancer survivors if they informed them about sperm banking before starting cancer therapies.”
A free, fast service
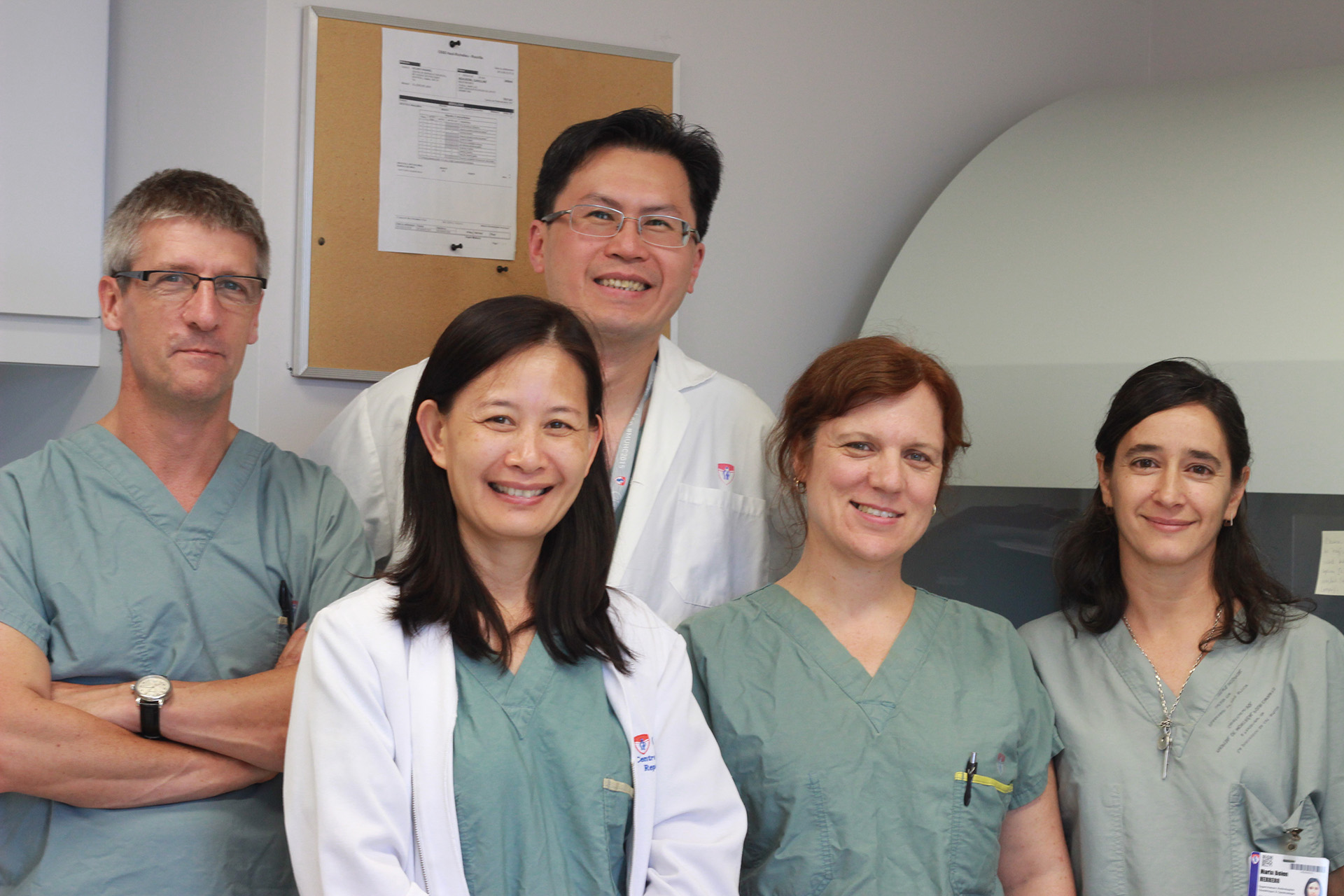
A patient’s decision to use sperm cryopreservation after a cancer diagnosis depends not only on counselling, but also on the costs associated with the collection and storage of samples. A recent study conducted by María Belén Herrero, PhD, chief andrologist at the MUHC Reproductive Centre, in collaboration with Dr. Chan and Dr. William Buckett, medical director of the MUHC Reproductive Centre, showed that since 2010, when fertility preservation became free for cancer patients as part of the Quebec’s public funding for assisted reproduction technologies (ART), patients have been willing to return for more sessions of sperm banking.
“The sperm banking procedure is covered by RAMQ and it is quick and easily accessible,” says Herrero.

Another study, also conducted by Herrero, Dr. Chan and Dr. Buckett, demonstrated that cancer survivors who had banked sperm and used it in fertility treatments later on presented at least similar reproductive outcomes as the population who used the sperm bank but didn’t have cancer.
“These results highlight the importance for healthcare professionals in oncology to discuss with patients the potential impact of cancer treatments on fertility and the benefits of fertility preservation,” she says.
A baby for a cancer survivor
After his successful cancer treatment, Greg Star continued his graduate studies in Pathology – he now works in sales for a biotechnology company – and he got married. But perhaps the sweetest part to Star’s story is he is also a father.
“The happiest part of my day is when I wake up in the morning and get to play with my son Thomas, who was born nine months ago,” Star says. “I didn’t know if I was going to be fertile or not after my treatments. Fortunately, I was. But if I wasn’t, I see making the choice to freeze my sperm as a younger man was the best insurance policy for happiness there is.”