Improvement, empowerment, autonomy: Physiotherapists aim at getting COVID patients back on their feet

|
Physiotherapists are Master’s trained healthcare professionals who play a significant role in the treatment of injury and disease with the ultimate goal of returning patients to their previous level of functioning. The physiotherapy profession relies on a clinical decision-making process that encompasses the integration of the best available evidence, the physiotherapist’s own clinical expertise and the values and needs of the patient receiving the care. This clinical decision-making process has never been so much put to the test as during the COVID-19 pandemic. Physiotherapists, as other professionals, are learning about the impact of the disease on mobility, function and recovery as they assess and treat patients. They have risen to the challenge, as highlighted in this interview. I want to personally thank all the physiotherapists of the MUHC for their initiative, courage and leadership in order to ensure patients receive the care they require. I am so very proud and honoured to have each and every one of you as members of the Multidisciplinary team. Kudos to all of you. Antoinette Di Re, Director of Multidisciplinary Services (adult sites), the Mental Health Mission and responsible for the NSA/SAPA trajectory. |

We virtually sat down with members of the physiotherapy team at the Glen site to talk about their work with COVID-19 patients. They were very generous with their thoughts, vision and passion for their work during these difficult times – and we hope you will be inspired as well.
Thank you to the entire COVID physiotherapy team:
Patricia Barassi, Suma Das, Angela Di Girolamo, Timothy Ho, Giuseppe Pazienza, Maria Pourasadi and Angelo Simonelli.
HOW DOES PHYSIOTHERAPY HELP COVID PATIENTS RECOVER?
Our goal in physiotherapy with the recovery of COVID patients is to prevent general deconditioning as much as possible. We have made handouts with general exercises and helpful recommendations for patients to maintain their physical functioning. We are involved with a very specific set of clients that require chest physiotherapy. This involves ensuring people’s airways become clearer of secretions.
Most importantly, we assess and monitor patients’ activity, tolerance and work of breathing with exercise and mobility in order to appropriately inform the medical and nursing teams what to expect from their patient functionally and how far they are from their baseline. As part of the multidisciplinary team, we help determine appropriate plans for our patients once they have surmounted their acute condition.
WHAT ARE THE SIGNS THAT TELL YOU YOUR WORK HAS A POSITIVE IMPACT ON THE PATIENT?
We know we can bring a positive impact to the patient when see a daily progression in their level of functioning, their physical improvement on assessment and mostly, seeing them smile every time they work with us. We are always most happy to get them back home safely to their loved ones, and seeing patients leaving to go to rehabilitation, which is the next stage of their process to recovery.
The reality is that a lot of hospitalized patients are greatly affected by COVID. Sadly, some of our patients cannot communicate, whether it be due to pre-hospital state (i.e. dementia, pre-existing comorbidities requiring long-term care) or sequelae from infection (altered mental status, weakness, confusion). However, in some cases, the family has expressed how much it means to them for us to be treating and caring for their loved one.
Many patients have a long way to go in terms of their medical course and rehabilitation. However many perseveringly and sometimes begrudgingly put in as much hard work as they can during the physiotherapy session. While some do not say anything about our help necessarily, they hope for results, others are only happy once they meet their goals! If patients are able to communicate, they are grateful and thankful for our care and expertise. They often talk of our patience and are happy to have us be part of their team.
HOW DID YOU ADAPT TO A NEW WAY OF WORKING?
The COVID crisis had most of us going through a tremendous amount of change. As physiotherapists, we had to change wards and work with teams we were not necessarily used to. Also, the added daily anxiety and amount of time it takes for proper donning and doffing PPE, making sure our hand hygiene was on point and hoping that we will not be bringing any of the virus home.
We had to become updated to the minute about how COVID affects a person physically and make sure we knew how to treat our patients appropriately for this new problem with a very unknown course.
The hardest part is being asked multiple times per day, by multiple professionals on multiple teams if we believe our patient has potential to improve and a lot of times not knowing because of the unknown nature of this virus.
We are not allowed to bring much equipment into the rooms and getting a second person to help out with difficult mobility is hard to come by. We also can no longer use the patient gym which is a detriment to our higher functioning population.
In addition, going in to check on a patient’s general status is no longer an easy task. Just chatting to see how they are doing is very difficult from behind the glass or if the patient will not or cannot answer the phone.
We have changed the method by which we assess and treat our patients. We are confined to their room and are unable to truly push their capacity for activity. This makes it more difficult to progress and less stimulating for our patients.
Also, disposition planning has become a nightmare. There are day-to-day changes as to which centres will accept our COVID positive patients. Even patients going back to their own residences have seen roadblocks as the criteria change on a daily basis and this is whether or not they are positive or negative. The CLSCs are having a difficult time accommodating for some of our patients increased needs as well. In addition, patients returning home have a lot to deal with coordinating who can take care of them and whether they are at risk of spreading the virus.
A major concern has been the status of our patient throughout the progression of the disease. In our experience, the virus often has an unpredictable course that can lead to a sudden deterioration which leaves us wondering if this sudden declining status is irreversible. It’s a demotivating and worrisome spot to be in. The inability to predict some of our complex patients’ potential has been quite hard for all of us regardless of our experience as we consider this the expertise of physiotherapists.
A PHYSIOTHERAPIST’S DAY: WHAT DOES IT LOOK LIKE?
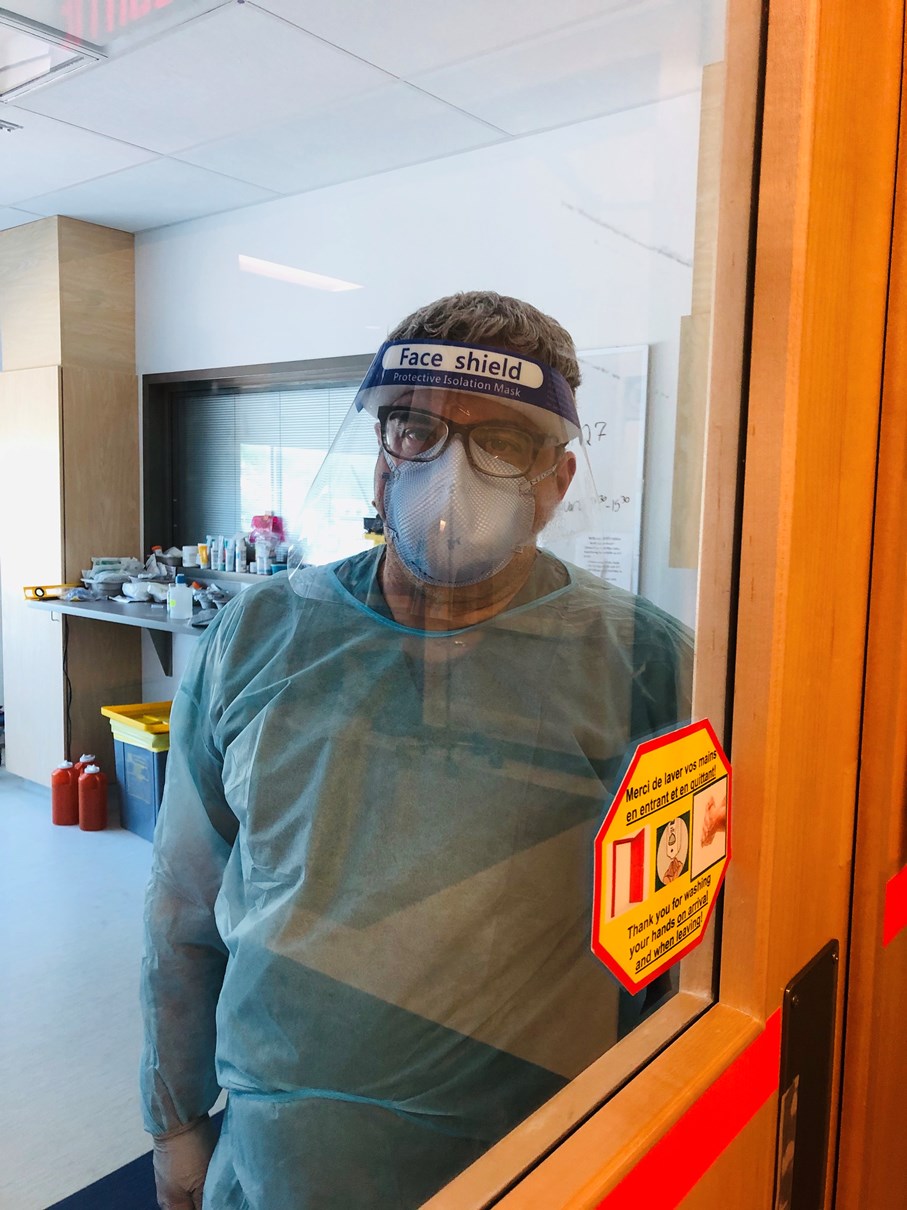
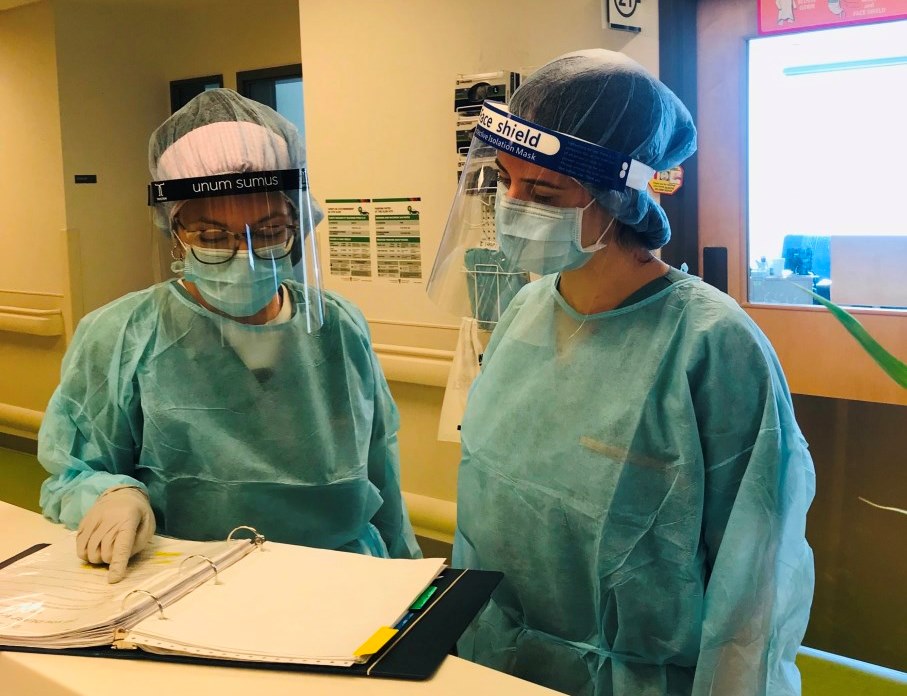
Our day starts with getting changed into scrubs, the uniform of the COVID wards, to make sure we minimize contamination outside the hospital. We bring up carts to one of the wards to ensure that we have proper face shield disinfecting stations. We round every COVID unit to check for new consult forms which means new patients that the COVID physio team would have to see.
We have a group chat where the 6 of us keep each other up to date and we try to make sure the work is split evenly and that one of our other team members is not alone so we can spot their hand hygiene and PPE don/doffing. We attend daily multidisciplinary rounds where we participate in the patient’s care plan. We discuss with nurses and PABs about each patient’s ability to participate in activity or any changes we see from day to day. Each individual patient we see takes a lot longer, not only because of the hygiene part of it but also because of the work that needs to be done outside the room to get that patient’s story.
We try to make sure everyone is getting the same care they would get if they were not COVID positive. We meet once or twice per day to make sure that we stay updated with policies, help each other through problems that arise and often just to support each other. We often leave later to make sure we are properly decontaminating prior to leaving the hospital.