
Cognitive Behavioural Therapy
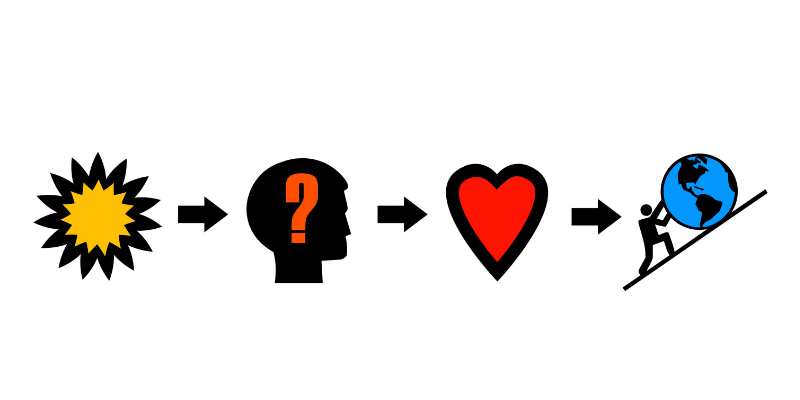
Cognitive Behavioural Therapy (CBT) is a type of psychotherapy. It is based on the idea that there is an interaction between how we think (cognition), feel (emotion/physical sensations) and act (behaviour).
CBT can be helpful in treating many mental disorders, including:
- depression
- anxiety disorders: panic, agoraphobia, social anxiety, generalized anxiety, illness anxiety, specific phobias
- obsessive compulsive spectrum disorders: obsessive compulsive disorder, habit disorders, tics
- trauma and stressor related disorders
- sleep disorders
- schizophrenia spectrum disorders and bipolar disorders, in combination with medication

The MUHC’s Centre for Cognitive Behavioural Therapy Research, Training and Intervention (CBT-RTI) is a centre of expertise on CBT.
We provide individual and group therapy.
 Learn more
Learn more


We are an interdisciplinary team of psychiatrists and psychologists, and trainees from various disciplines, including psychiatry, psychology, nursing and occupational therapy.
 Learn more
Learn more

We are located at the Allan Memorial Institute.
To become a patient at the Centre for CBT-RTI, you need a referral from a healthcare professional.
 How to reach us
How to reach us
