SipSup nutrition program finds momentum across MUHC
After a successful implementation in the Department of Internal Medicine of the Montreal General Hospital (MGH-MUHC) in 2016, a program to improve the nutritional status of patients is being carried out in the same service at the Royal Victoria Hospital (RVH-MUHC).

Nutritionists Deborah Fleming and Ann Coughlin have high hopes for the implementation of the SipSup program across all MUHC sites by fall 2018..
With the SipSup program, nurses give a small volume of a nutritionally dense supplement to malnourished or at risk patients twice a day, at the same time as they administer medication.
“We know that patients are more likely to drink supplements when they are given at the same time as the medication by nursing,” says Deborah Fleming, MUHC manager of Clinical Nutrition (adult sites).
Getting the nurses onboard is one of the essential success factors for the program. Another key element is providing the right supplement at the right time.
- Supplements are served in a small portion (half a cup or 115 mL) so patients still have enough appetite to eat their food.
- They can be served as either a liquid, for patients who can eat regular textures, or as a pudding, for patients who have difficulty swallowing.
- Each portion gives patients an extra 9 grams of protein and 220 calories, to help repair, build and maintain cells and body tissues.
- They are vanilla-flavoured – universally preferred – and are served in attractive packaging.
The impetus behind the project stemmed from the results of a study done at both the MGH and the RVH to determine the extent of malnutrition or the risk of malnutrition of patients during admission as compared to published findings in other hospitals. It was determined that 42 per cent of patients admitted to Internal Medicine at the MGH were at risk of being malnourished or suffering from malnutrition. At the RVH, the rates were even higher – 50 per cent.
A collaborative effort
The SipSup project at the MGH
Nutritionist Helena Caravolas-Karasek
Nurse Manager Nancy Plaisir
Pharmacist Louise Papillon-Ferland
Nursing staff at the Department of Internal Medicine
The SipSup project at the RVH
Nutritionist Sarah McDonald Pauletto
Nurse Manager Aparna Bhattajarjee
Pharmacist Louise Papillon-Ferland
Nursing staff at the Department of Internal Medicine
Successful identification and treatment of malnutrition requires a multidisciplinary approach. Through the combined efforts of the Nursing, Nutrition and Pharmacy departments, the SipSup program has demonstrated that patients are able to consume at least 75 per cent of the food on their meal tray as well as consume the supplement at medication times.
“Besides excellent patient compliance, we also received very positive feedback from nursing,” says Ann Coughlin, assistant manager of Clinical Nutrition (adult sites). Before the end of 2018 the plan is to introduce the SipSup program to the other services across the adult sites of the MUHC. And to allow the program to continue its expansion, Deborah and Ann are in the process of implementing systematic nutritional screening across the MUHC.
“Evidence shows that early nutrition intervention can reduce complication rates, length of hospital stay, readmission rates, mortality and cost of care. Screening allows us to flag at-risk patients and enroll them in SipSup as soon as possible.”
SipSup is so successful that other hospitals in Montreal, Quebec and other cities across Canada have expressed interest in learning more about it.
Eating well in the hospital and at home
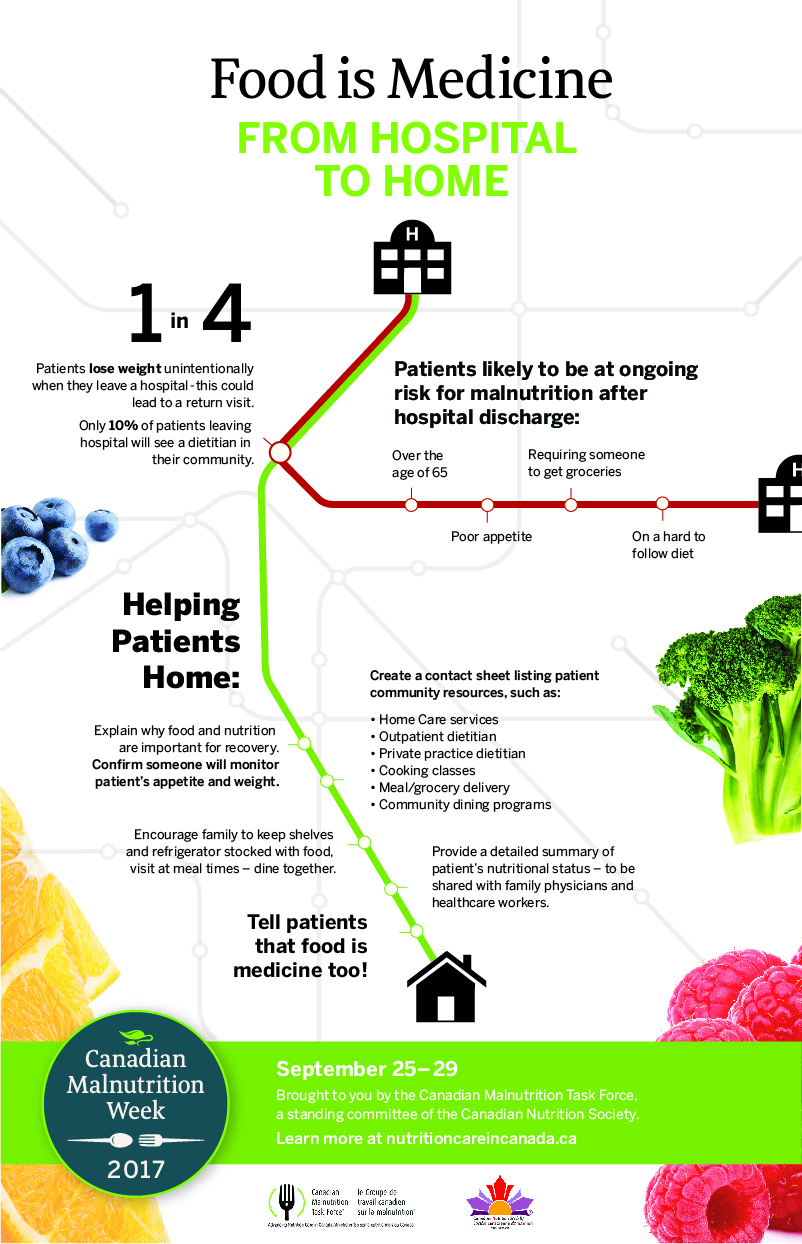
“From hospital to home” is the theme of the third edition of the Canadian Malnutrition Week (September 25 – 29). MUHC nutritionists invite members of inter-professional teams to think of ways they can help patients meet their nutritional needs in the hospital, and how they can go home with tools to meet their nutritional needs.
Patients who don’t eat properly are twice more likely to be readmitted in the healthcare system. According to the Canadian Malnutrition Task Force™, the total annual burden of malnutrition in Canadian hospitals is approximately $2 billion.
“Discharged patients are still in a phase of recovery and need to eat well to heal,” says Deborah Fleming, MUHC manager of Clinical Nutrition (adult sites). “As a hospital, it is important to reduce rates of readmission of malnourished patients, and if they don’t return, we’ve done our job.”