Partner Clinics Project: a winning alliance
A new initiative linking the McGill University Health Centre (MUHC) and five family medicine groups in Montreal is facilitating care for those living with chronic conditions.

The Partner Clinics Project Team
The Partner Clinics Project, an initiative brought forward by the Ministry of Health, aims to ensure that MUHC patients living with chronic diseases have the opportunity to be registered quickly with a family doctor close to home. Through the Guichet d'accès pour la clientèle orpheline (GACO), the project is proposing an effective alternative for patients visiting specialists for non-complex care.
The initiative was put into motion in 2015, and will be underway for the next four years. The project currently focuses on patients living with conditions such as chronic obstructive pulmonary disease (COPD), asthma, cardiac problems (hypertension, insufficiency) diabetes and blood disorders (anticoagulation therapy). Efforts have also been made to include cancer survival patients who don’t have a family physician.
Ensuring success
Looking for a family doctor? Follow the link below to register your name on the government’s official waiting list. All requests are evaluated and prioritized according to health.
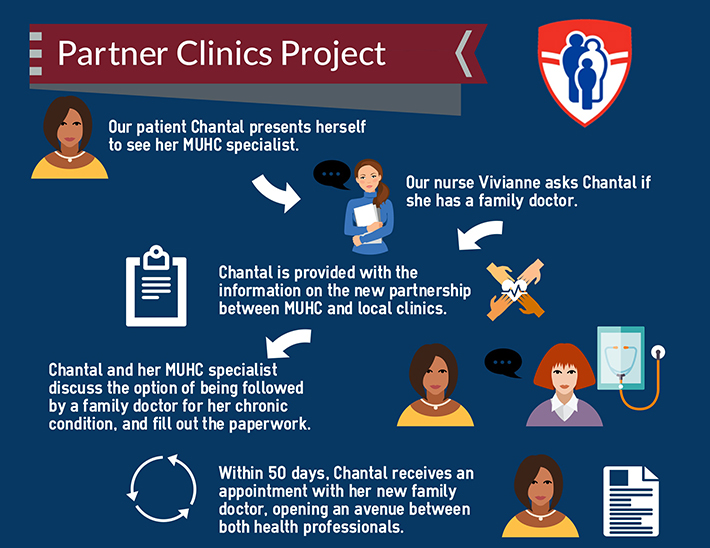
The Partner Clinic Project involves collaboration from staff on every level. When a patient presents themselves at the clinic, the clerical staff and nurses work to identify their eligibility, starting with the basic question: Do you have a family physician? The triage is based on a list of pre-determined clinical criteria and where the patient lives. If they are a fit for the project, patients are provided with information explaining the new program.
The relationship between patient and specialist is an important part of the process. The specialist discusses the opportunity with the patient and ultimately makes the decision to draft up a referral; keeping the patient’s wellbeing at the forefront. Once the referral reaches GACO, patients should receive an appointment with a family doctor in one of the partner clinics within 50 days.
THE ROLE OF A FAMILY DOCTOR
Family doctors play a very significant role in a patient’s life. Kathy Riches, a nurse clinician who works at the Montreal Chest Institute of the MUHC, focuses on asthmatic patients. She explains why the care and expertise of a family doctor cannot be replaced by a specialist, especially for those living with a chronic condition:
In my everyday work as a clinician it is very important for me to see that patients have family doctors to ensure that they receive comprehensive care. They [family doctors] fill in the gaps of things we're not doing here at the MUHC, and address some of the comorbidities that can affect asthma. Gastric reflux, obesity, as well as stress and anxiety are all examples. It’s extremely important to have a global approach. The patients are reassured by that, there’s a physician that sits down and talks to them about everything that's going on.
Patients who fall outside of the geographic parameters of the project are not forgotten. Nurse clinicians at the MUHC make it a priority to help patients through the process of finding a family doctor. Kathy says that the initiative has provided her with the tools to help point the patients she sees in the right direction.
“No matter what,” she says, “it helps meet patients’ needs.”
Dr. James Martin, chair of the Department of Medicine of McGill University, and physician-in-chief of the MUHC, says that while the project comes with its challenges it is a good concept. It could benefit patients and help them better manage their conditions.
“This could create the possibility of intervening before their health condition deteriorates, which would require them to return to the hospital,” he says.
The right patient, at the right place, at the right time
The notion of prevention is a key factor that plays into the overall objective of the project. Nurse Clinician Kathy Riches says that the screening by a family doctor is an important component to preventative care. This erases the idea that a visit with a specialist can replace a check-up with a family doctor.
“It is about having the right patient, at the right place, at the right time; making the process easier and more efficient for all involved,” says Project leader and Assistant to the MUHC Director of Professional Services Carole Lapierre. “Considering the alliance that will grow over time between the family physicians, the GMF interdisciplinary teams and the MUHC specialist teams, we believe that we are working toward an essential combination of care for our community—a way to ensure that our patients are in good hands.”
Once a patient is referred to a family doctor, this does not signal an end to their relationship with the MUHC. Conversely, it paves a corridor between the different lines of health care. The current goal is to have 1,000 patients referred per year; a goal Carole believes is attainable with all hands on deck.
“There is a lot of opportunity in this project,” she says, “I hope that in six months we will be able to present very encouraging results.”
Patient testimonial: Cheryl-Anne
When Cheryl-Anne began to feel ill, she knew something wasn’t right so she booked an appointment with her family doctor. “After discussing my symptoms, he advised that I be seen by a specialist,” she says. “I was eventually diagnosed with chronic leukemia.”
Cheryl-Anne counts herself lucky, as she was put on a new type of medication that worked well as a treatment. However, as with any medication, it is important to be followed to not only assess the efficacy, but also manage any possible side effects that may occur. For patients with chronic conditions, it is sometimes difficult to differentiate between symptoms caused by their condition or symptoms from their medication. That is why Cheryl-Anne says that despite seeing a specialist, it was important for her to stay in contact with her family doctor. It gave her an overall outlook on her health; all while saving her a visit to the hospital when her family doctor could provide the necessary follow-ups. She found herself working with both her specialist and family doctor to manage her condition, creating a link between the two.
For Cheryl-Anne, this link between the different lines of health care allowed her to comfortably take charge of her health condition; as she herself became a mini-expert on chronic leukemia and its effects. The Partner Clinics Project hopes to create that feeling of empowerment and control for other patients living with chronic conditions, ensuring they receive a complete circle of care.
