As technology evolves, so does patient care in Cardiac Electrophysiology at the MUHC
The team of the Electrophysiology Laboratory has to be up to speed with the rapidly evolving technology in cardiovascular care.
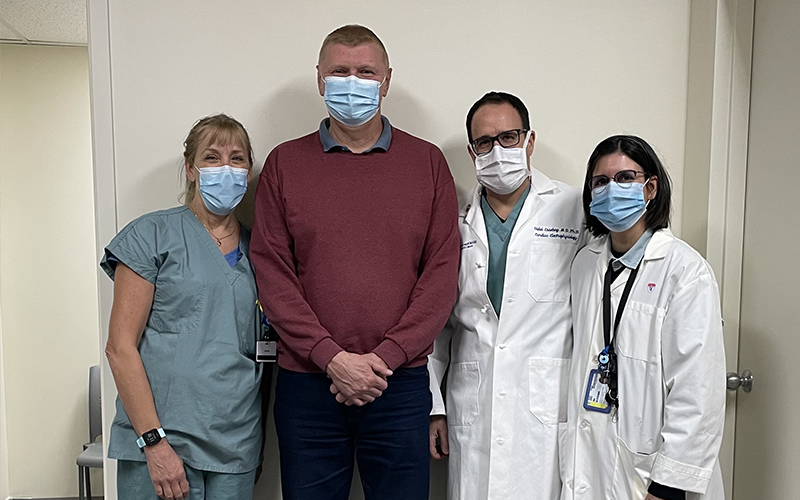
Vladimir Grishin’s life changed for the better the day he stepped into the Cardiac Electrophysiology Laboratory at the McGill University Health Centre (MUHC) and agreed to be part of a clinical trial coordinated via the Research Institute of the MUHC (RI-MUHC), a first of its kind in Quebec to treat his atrial fibrillation problems.
As a 52-year-old man with a history of arrhythmia (irregular heart beat), he had already undergone a somewhat simpler procedure for the right atrium (or right upper chamber of his heart), which was successfully ablated in 2014. However, since 2020, he began to suffer from a new type of arrhythmia, atrial fibrillation, originating from the top left side of his heart.
“Arrhythmia is a terrible disease, you feel dizzy, you can’t move too much. It was a very hard time for me; sometimes the episodes occurred as many as 14 times a month. For almost a year, I was weak and I couldn’t sleep well because the heart did not beat normally. That’s not life!” notes Mr. Grishin.
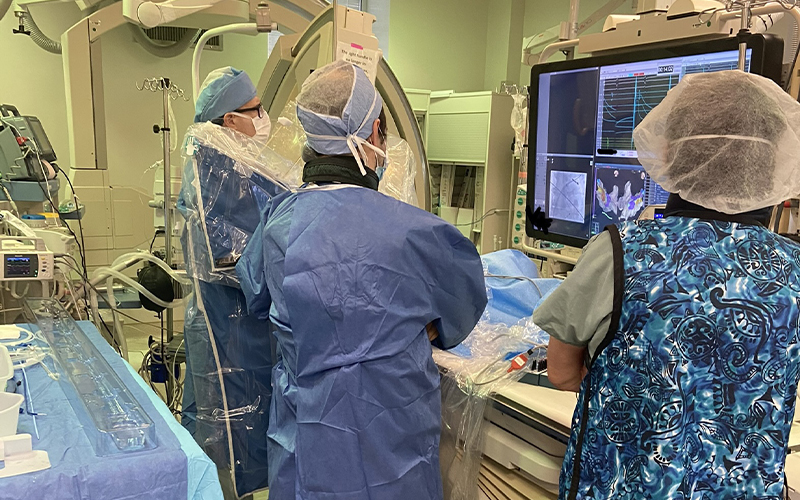
Ablation creates scars in the heart that stabilize the electrical short circuits. The research trial was intended to assess a new type of ablation therapy, the PulseSelect™ Pulsed Field Ablation (PFA) System. This new minimally invasive procedure was developed by Medtronic and pre-approved by Health Canada for clinical use. Also called atrial fibrillation (AF) ablation, it uses a catheter to deliver pulsed electric fields, a novel type of energy source to treat AF. While the currently approved catheters use either radiofrequency (burn) ablation or cryo (freeze) ablation, pulsed field ablation or electroporation interrupts irregular heart rhythms and also reduces undesirable damage to the surrounding tissues.
“By preventing long-term complications of atrial fibrillation such as stroke and heart failure, ablation has the potential to improve health, and reduce the use of healthcare resources and hospital admissions,” says Dr. Vidal Essebag, medical director of Cardiac Electrophysiology at the MUHC. Dr. Essebag performed the procedure on Mr. Grishin at the Cardiac Electrophysiology Laboratory of the Montreal General Hospital (MGH) in October 2021. The procedure was a success, and the patient was able to return home the next morning.
“After a week, I think I was ready to run a marathon,” jokes Mr. Grishin. “I appreciated greatly the treatment, the team and their professionalism,” he says.
“From the patient’s perspective, it was very well tolerated,” says Dr. Essebag. “It’s encouraging to know that in the future, a growing number of patients will be able to benefit from this procedure as it becomes more effective and safer.”
Atrial Fibrillation (AF)
- AF is the most common heart rhythm disorder
- More than 350,000 people are diagnosed annually in Canada; this number is projected to grow to more than 1 million by 2050
- AF poses an increased risk of blood clots, stroke, heart failure and death
New generation pacemaker improves treatment of heart failure
The Cardiac Electrophysiology team is also keeping up to speed on the use of state-of-the art pacemakers. Last July, a patient with severe heart failure became the first in Canada to undergo a successful implant of a pacemaker and Cardiac Resynchronization Therapy (CRT) equipped with advanced new software. The procedure took place at theCardiac Electrophysiology Laboratory at the Glen site.
“When the patient came in, her heart failure was so severe that it was less than half the normal heart function. She also suffered from severe arrhythmia causing heartbeats that were either dangerously too fast or too slow, as well as an electrical conduction abnormality causing loss of synchrony of heart contraction and contributing heart failure. Weeks later, her heart function had returned to completely normal.”
Also made by Medtronic, the Percepta™ Cardiac Resynchronization Therapy (CRT) pacemaker features improved software algorithms that allow the device to fine-tune itself continuously.
“It’s like comparing an iPhone 11 and an iPhone 13 pro. Their size is the same and you dial the number the same way, but the device and the algorithms it uses are more sophisticated and can do a better job at preventing a slow heartbeat and resynchronizing heartbeats,” says Dr. Essebag.
Dr. Essebag praises the Cardiac Electrophysiology team, who must constantly adapt to the rapidly evolving technology.
“We are fortunate to have a truly outstanding team. They are always open to learning new procedures. Most importantly, they take our patients’ wellbeing to heart and are always tuned in to their needs.”
The Cardiac Electrophysiology Laboratory at the MGH and the Cardiac Electrophysiology Laboratory at the Glen site received financial support from the MGH Foundation and the MUHC Foundation, respectively.

Front, left to right: Bernard Soucy, Antonella Cantera, Natalie Bourne
Second row, left to right: Hasan Gholami, Peggy Vehoef, Vidal Essebag, Stephanie Doray
Back, left to right: Daniel Donnici, Francesco Donatelli, Noushin Bayat, Louise Kezerle, Eric Lafontaine

Front, left to right: Noushin Bayat, Yoel Bitton, Vidal Essebag, Julie Laliberté, Stacey Mooney, Renée Bienkowsky, Stéphanie Martin
Back, left to right: Julie Guimond, Vincent Piché-Roy, Kerwin Chahal