Study confirms efficiency of app that quickly assesses risk of cancer predisposition syndromes in children with cancer
Cancer predisposition screening tool MIPOGG was developed at the Montreal Children’s Hospital and SickKids
Montreal, — About one in every 10 pediatric cancer patients has a cancer predisposition syndrome (CPS)—an underlying genetic disease that predisposes the child or youth to develop a cancer. Yet, as important as it is for cancer management and surveillance, diagnosing a CPS remains a challenge. A new study by a team of researchers at the Research Institute of the McGill University Health Centre (RI-MUHC), the Montreal Children’s Hospital and The Hospital for Sick Children (SickKids) shows that a free and easily accessible eHealth tool called MIPOGG (McGill Interactive Pediatric OncoGenetic Guidelines) is able to differentiate between a low or high likelihood of having a CPS in children and youth with cancer. The study, published today in JAMA Oncology, validates MIPOGG as the only eHealth CPS screening tool in pediatric oncology that has completed a series of performance assessments establishing its diagnostic accuracy measures.
Diagnosing a child or youth with a CPS is important to adjust the patient’s current cancer treatment, offer screening to family members and consequently, provide cancer surveillance services to detect new cancers faster. With over 100 known CPSs that can lead to cancer in children and adolescents and no standardized way of evaluating the risk of a CPS in children and youth with cancer, it is often difficult for doctors to know which of their patients has an underlying CPS.
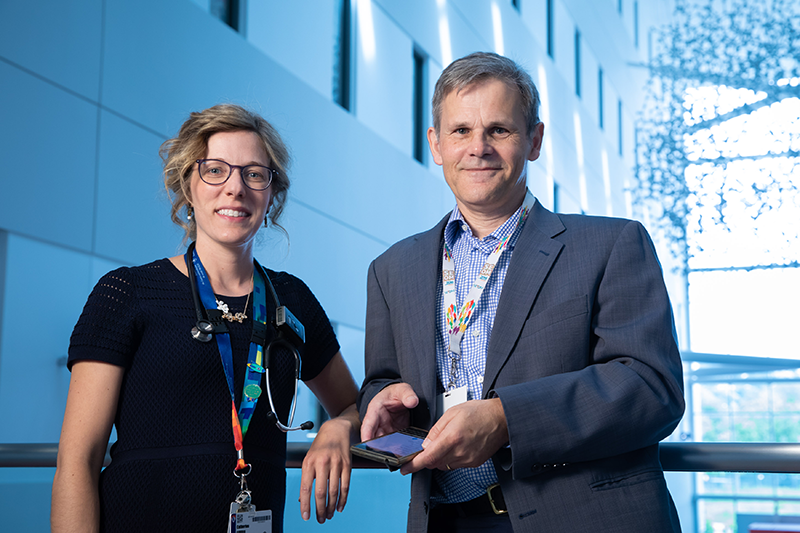
“A CPS diagnosis requires clinician expertise, access to genetic testing and result interpretation. While some large academic hospitals have the capacity to offer genetic testing to every single patient in oncology, most hospitals are not able to offer genetic evaluations to all (or any of) their patients,” explains Dr. Catherine Goudie, Pediatric Hematologist-Oncologist at the Montreal Children’s Hospital and a researcher in the Child Health and Human Development Program at the RI-MUHC.
“MIPOGG answers a real need, as it allows doctors to quickly identify children who are at greater risk of having a cancer predisposition syndrome and better identify those who can benefit from genetic testing,” she adds.
Based on an idea by Dr. Goudie and Dr. William Foulkes, Clinical Cancer Geneticist and Senior Scientist in the Cancer Research Program at the RI-MUHC, MIPOGG uses decisional algorithms to analyze patient data, as well as personal and family histories, in order to find recognized associations with specific CPSs. When necessary, it generates a recommendation to request a genetic evaluation to confirm the presence of a CPS. Its scientific development is the result of five years of work, involving a team of researchers and students led by Dr. Goudie, Dr. Foulkes, and Dr. David Malkin, Senior Staff Oncologist and Senior Scientist in the Genetics & Genome Biology research program at SickKids. Already used by over 800 health professionals and students in more than 50 countries, MIPOGG is available as a free app in English and French and works with all cancer types in children and youth.
“Clinical decision-making tools that can help support potential early diagnosis of cancer are critical to the future of individualized medicine, and our ability to not only improve patient outcomes but also support children, youth and families on their care pathways from day one,” says Dr. Malkin, Co-Lead of the Precision Child Health initiative at SickKids.
In this international study, the researchers evaluated MIPOGG’s performance in more than 1,000 children and youth with cancer across 15 sites. After using MIPOGG to perform a retrospective assessment of the patients’ data and family histories, they found that the tool was able to rapidly identify children and youth at high risk of having a CPS.

“MIPOGG correctly recommended 99.5 percent of patients with a CPS for genetic evaluation. In addition, all patients who subsequently developed a second cancer were identified at an earlier time point than they were by healthcare practitioners,” says Lara Reichman, a genetic counsellor at the MUHC and a co-author of the study.
The team also assessed the actual measurement properties of MIPOGG by comparison to extensive genetic sequencing in oncology patients. MIPOGG demonstrated a highly favourable diagnostic accuracy profile: children who scored positive on MIPOGG had a 17.6 percent chance of having a CPS (positive predictive value), and those who scored negative had a 98.6 percent chance of not having a CPS (negative predictive value). Additionally, 90.7 percent of patients who had a CPS found via genetic sequencing were identified by MIPOGG as being at high risk.
“One problem with testing lots of genes in children with cancer is that not all the alterations identified actually cause the cancer,” explains Dr. Foulkes. “MIPOGG can also help here, as it usually only identifies truly causal associations between altered genes and the cancer. Therefore, it can also help prioritize and rationalize healthcare resources in cancer genetics.”
In another study, recently published in the Journal of Clinical Oncology, the team of researchers had shown that MIPOGG can help predict which childhood cancer survivors may be at risk of developing other cancers later in life. With this new study, they provide evidence that MIPOGG actually does what it’s meant to do, i.e., correctly identifying CPSs that are causal of a child’s cancer.
About the study
The study Performance of the McGill Interactive Pediatric OncoGenetic Guidelines for Identifying Cancer Predisposition Syndromes was conducted by Catherine Goudie, Leora Witkowski, Noelle Cullinan, Lara Reichman, Ian Schiller, Melissa Tachdjian, Linlea Armstrong, Katherine A. Blood, Josée Brossard, Ledia Brunga, Chantel Cacciotti, Kimberly Caswell, Sonia Cellot, Mary Egan Clark, Catherine Clinton, Hallie Coltin, Kathleen Felton, Conrad V. Fernandez, Adam J. Fleming, Noemi Fuentes-Bolanos, Paul Gibson, Ronald Grant, Rawan Hammad, Lynn W. Harrison, Meredith S. Irwin, Donna L. Johnston, Sarah Kane, Lucie Lafay-Cousin, Irene Lara-Corrales, Valerie Larouche, Natalie Mathews, M Stephen Meyn, Orli Michaeli, Renée Perrier, Meghan Pike, Angela Punnett, Vijay Ramaswamy, Jemma Say, Gino Somers, Uri Tabori, My Linh Thibodeau, Annie-Kim Toupin, Katherine M. Tucker, Kalene van Engelen, Stephanie Vairy, Nicolas Waespe, Meera Warby, Jonathan D. Wasserman, James A. Whitlock, Daniel Sinnett, Nada Jabado, Paul C. Nathan, Adam Shlien, Junne Kamihara, Rebecca J. Deyell, David S. Ziegler, Kim E. Nichols, Nandini Dendukuri, David Malkin, Anita Villani and William D. Foulkes
Funding for the development of MIPOGG and for this study was provided by the Montreal Children’s Hospital Foundation, Cedars Cancer Centre / Sarah's Funds for Cedars, SickKids Foundation, Pediatric Oncology Group of Ontario (POGO), Canadian Institutes of Health Research (CIHR), Fonds de recherche du Québec—Santé (FRQS), Cancer Research Society, TD Ready Challenge/TD Bank, Fondation Charles-Bruneau, Garron Family Cancer Centre—Great Cycle Challenge and Cole Foundation.
About the Montreal Children’s Hospital
Established in 1904, the Montreal Children’s Hospital (MCH) is Quebec’s oldest children’s hospital and the pediatric hospital of the McGill University Health Centre (MUHC). A tertiary and quaternary care teaching and research facility, treating newborns, children and adolescents up to age 18, it serves 63% of the geographic population of Quebec.
With its pediatric care and research facilities adjacent to the adult facility on the Glen site, the Children’s is in a unique position to offer services and research across the lifespan. The Centre for Innovative Medicine—the only clinical research centre in a hospital setting in North America—allows its researchers to conduct clinical trials on the Hospital site.
The Children’s is a leader in providing a broad spectrum of highly specialized care to young patients and families from all across Quebec. The hospital is a provincially designated trauma centre and is recognized for its wealth of expertise in cardiology and cardiac surgery, emergency care, neurology and neurosurgery. thechildren.com
About The Hospital for Sick Children (SickKids)
The Hospital for Sick Children (SickKids) is recognized as one of the world’s foremost pediatric health-care institutions and is Canada’s leading centre dedicated to advancing children’s health through the integration of patient care, research and education. Founded in 1875 and affiliated with the University of Toronto, SickKids is one of Canada’s most research-intensive hospitals and has generated discoveries that have helped children globally. Its mission is to provide the best in complex and specialized family-centred care; pioneer scientific and clinical advancements; share expertise; foster an academic environment that nurtures health-care professionals; and champion an accessible, comprehensive and sustainable child health system. SickKids is a founding member of Kids Health Alliance, a network of partners working to create a high quality, consistent and coordinated approach to pediatric health care that is centred around children, youth and their families. SickKids is proud of its vision for Healthier Children. A Better World.
About McGill Interactive Pediatric OncoGenetic Guidelines (MIPOGG)
MIPOGG is an app that identifies children at higher risk of cancer predisposition syndromes in pediatric oncology. These syndromes are recognized as an important cause of pediatric cancer development. Health professionals who manage children and adolescents with cancer have a unique opportunity to identify these patients and their families for genetic evaluation. This task is increasingly challenging for clinicians as the knowledge of cancer genetics is growing at a rapid pace. Conceptualized by Dr. Catherine Goudie and further developed via the collaboration of the Montreal Children’s Hospital of the McGill University Health Centre and The Hospital for Sick Children (SickKids), with the support of numerous partners, MIPOGG offers access to simple tumour-specific algorithms that guide the clinician through the decisional process of whether a child requires a genetics referral. MIPOGG incorporates evidence-based educational modules outlining associations between pediatric tumours and cancer predisposition syndromes. mipogg.com
