The Unsung Heroes of Organ and Tissue Donation
The MUHC is one of the largest transplant centres in the province of Québec, and in 2024, 153 organ transplantations and 453 tissue transplantations were performed here. Behind every successful outcome, there is a vast network of over 100 healthcare providers working tirelessly to make it happen!

| We developed a detailed diagram showing the large number of people involved from the initial identification of a potential donor to the transplantation, and then, subsequent life-long follow-up. Doctors, surgeons, nurses, respiratory therapists, laboratory technicians, radiology technicians, physiotherapists, and nutritionists are all involved in the process... as well as other key figures which might surprise you. |
Coordinators working for Transplant Québec and Héma-Québec ensure that organs and tissues are matched to the best recipient. In Québec, volunteer police officers deliver organs and members of the surgical team to the right location and secure the entire transport process. Héma-Québec works with funeral homes whenever necessary to ensure the timely procurement of precious tissues.
The Donation Process
(1) Decision: The process begins with the decision to become a donor. This is done by signing the back of your RAMQ card, registering your choice on the RAMQ or Notary registry, and sharing your decision with your family.
(2) Donor Identification and Evaluation: Potential donors are identified. Their medical history is evaluated.
(3) Family Approach: If the patient meets the criteria to be an organ or tissue donor, the family is approached for consent to move forward with donation in accordance with the patient’s wishes.
(4) Matching Organ Donors with Recipients: A database is used to match donors with recipients based on blood type, size match, and urgency.
(5) Matching Tissue Donors with Recipients: Tissues don’t need to be matched in the same way as organs. Héma-Québec stores the tissues, some up to five years, and distributes them based on need. No recipient matching is needed as the tissues do not need blood and oxygen to function.
(6) Organ Recovery and Preservation: Once a match is found, the organs are surgically recovered and preserved for transplantation.
(7) Transplantation: The organs are transplanted into the recipients within hours of procurement. On the other hand, tissues are banked and released as they are needed.
(8) Recovery: After their organ transplant, the patient is brought to the ICU or the Transplant Unit, then sent home once they feel well enough. Recovery for tissue transplantation also involves a hospital stay.
(9) Follow-up: The organ transplant recipient comes to the clinic for regular check-ups with the post-transplant healthcare professionals and begins taking anti-rejection medications. Follow-up for tissue donation is simpler; anti-rejection medications are not needed, and clinic visits are much less frequent. The families of deceased donors are provided with resources and ongoing support to help them cope with grief.
The OTDT process is a testament to the dedication and collaboration of countless healthcare providers. It is important to appreciate the complexity of this life-saving work.
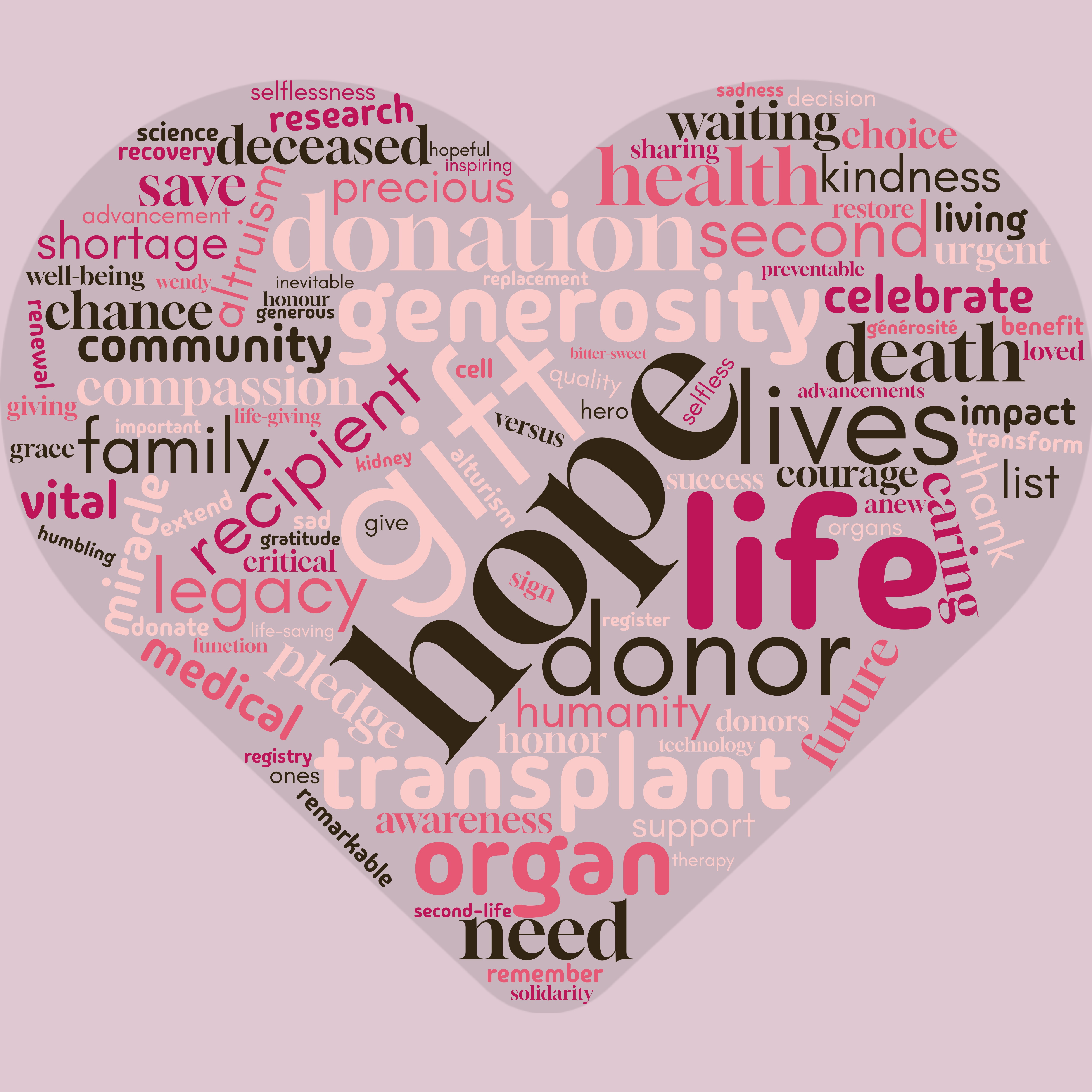
The word cloud below was created by the Multi-Organ Transplant and Donation Program (MOTDP) as a reminder of the hope and compassion that drives the process; we asked members to share a word that comes to mind when they think of donation and transplantation. The bigger the word, the more it was given as an answer. The resulting word cloud is a powerful visual.