Researchers find a possible therapeutic target in the “genetic landscape” of aggressive and deadly pediatric brain tumours
A new study reveals that PFA ependymoma brain tumours display unique 3D genome features that could be exploited therapeutically
Montreal, July 10, 2024—Posterior fossa group A (PFA) ependymoma are rare, treatment-resistant pediatric tumours of the central nervous system that originate in the brain and spinal cord. They have the highest recurrence rate and poorest prognosis of all childhood cancers, due to the lack of effective treatment.
Hope is on the horizon now that an international research team led by scientists at Baylor College of Medicine in Texas, USA, and the Research Institute of the McGill University Health Centre (RI-MUHC) in Montreal, Canada, have identified unique 3-dimensional features called TULIPs in the genome of PFA ependymoma that could eventually be targeted in the development of more effective therapies. The findings appear in Cell.
“PFA ependymomas are lethal. One of the reasons behind the little progress toward the development of effective treatments for these tumours is that the majority of PFAs lack clear genetic mutations driving tumour growth. Without a clear genetic target against which we could design specific therapies, we investigated another aspect of the tumour, how the DNA is packed inside the nucleus of the cell,” says senior and lead author, Marco Gallo, Associate Professor of pediatrics, hematology-oncology at Baylor and Texas Children’s Hospital.
“Our work was driven by a simple fact: PFA ependymoma are usually diagnosed in very young children, and have no efficient treatment. Radiation therapy, the only treatment currently available, is not effective and causes serious developmental and cognitive issues. That’s a reality we hope to change,” says Canada Research Chair in Pediatric Oncology Dr. Nada Jabado, co-senior author of the study, a Senior Scientist in the Child Health and Human Development Program at the RI-MUHC and a Pediatric Hemato-Oncologist at the Montreal Children’s Hospital of the MUHC.
Uncovering the 3D configuration of tumour cells’ genomes
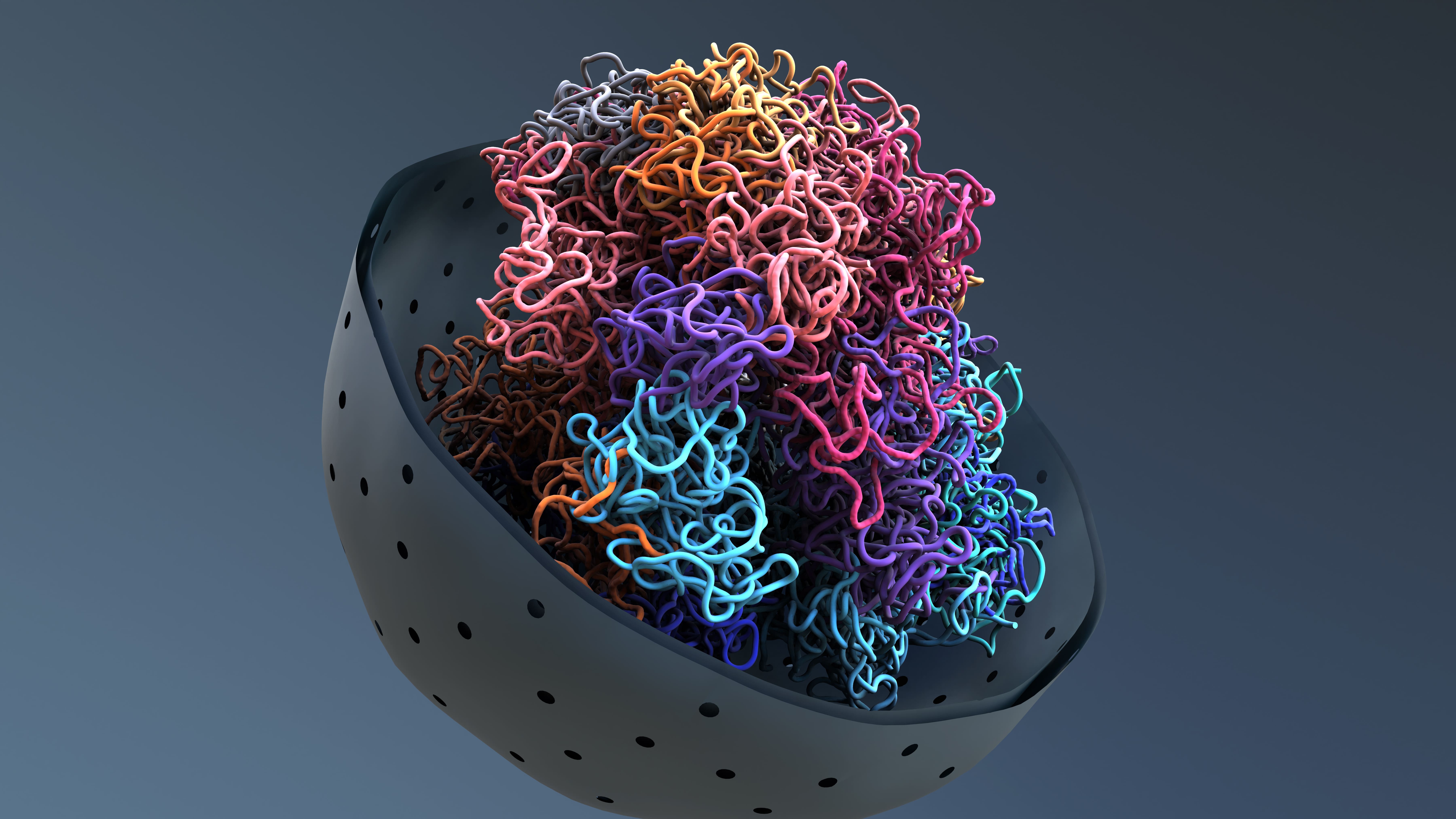 Every cell in the body has about 6.6 feet (2 meters) of linear DNA that is stored in its nucleus in a manner that enables the cell to easily access the genes it uses most often and set aside those less used. This would be like organizing the closet with the clothes most frequently used at the front and those rarely worn on the back. To fit in the tiny nucleus, the long DNA molecules are folded, twisted, looped, which results in specific 3D conformations, some tighter, some more relaxed, that can ultimately help the cell express the genes needed to do its job.
Every cell in the body has about 6.6 feet (2 meters) of linear DNA that is stored in its nucleus in a manner that enables the cell to easily access the genes it uses most often and set aside those less used. This would be like organizing the closet with the clothes most frequently used at the front and those rarely worn on the back. To fit in the tiny nucleus, the long DNA molecules are folded, twisted, looped, which results in specific 3D conformations, some tighter, some more relaxed, that can ultimately help the cell express the genes needed to do its job.
In this study, the researchers looked closely at what we might call the “geography” of the PFA ependymoma cell genome (the entire set of DNA instructions found in the cell).
“We investigated the unique ways PFAs cells organize their DNA in 3D, by orchestrating strong interactions between regions of the genome that are normally very far apart. We discovered specific regions that are not present in other types of pediatric brain cancer and that recur at predictable genomic locations. We named them TULIPs, for Type B Ultra-Long Interactions in PFAs,” says Dr. Michael D Taylor, co-senior author of the study and Professor of pediatrics, hematology – oncology and neurosurgery at Baylor and Texas Children’s. He also is the Cyvia and Melvyn Wolff Chair of Pediatric Neuro-Oncology at Texas Children's Cancer and Hematology Center.
The researchers used the Hi-C technology to profile the 3D architectures of the entire genomes of PFA tumours and compared them with those of a large cohort of samples from different tumour types and nonmalignant tissues. In the process, TULIPs appeared as specific regions of very tightly compacted, thus hard-to-access, DNA, a sign that the cell may not use the genes in that region often.

“TULIPs also tend to interact with each other over very long distances. A TULIP might be at the end of a chromosome and another TULIP at the other end of the same chromosome, and they find their way to interact with each other with surprising strength,” explains Prof. Gallo. “TULIPs on different chromosomes can also converge and strongly interact with each other. We also found that regions outside TULIPs appear more relaxed overall. This is important because TULIPs are linked to the cell’s function.”
A potentially actionable chemical tag
According to the study findings, TULIPs carry a methyl group on histone H3K9, a protein associated with DNA that can act as a chemical tag. Indeed, when the research team inhibited the tagging of H3K9 in PFA patient-derived cultures, they witnessed weaker interactions between TULIPs and impaired PFA cell survival. These observations suggest that TULIP interactions are important for PFA cell viability, opening up new potential targets for treatment.
“We believe that TULIPs are ephemeral structures present at an early stage of cancer development in progenitor cells - cells that descend from stem cells and precede the creation of mature cells, very early in life. However, more research is needed to understand the mechanism by which TULIPs arise and mediate cancer cells behaviour,” says Dr. Jabado, who is also a professor in the Department of Pediatrics at McGill University. “By further investigating this mechanism, we may be able to explore treatment strategies to remove them to promote tumour elimination.”
About the study
The study TULIPs decorate the three-dimensional genome of PFA ependymoma was conducted by Michael J Johnston, John JY Lee, Bo Hu, Ana Nikolic, Elham Hasheminasabgorji, Audrey Baguette, Seungil Paik, Haifen Chen, Sachin Kumar, Carol CL Chen, Selin Jessa, Polina Balin, Vernon Fong, Melissa Zwaig, Antony MichealRaj, Xun Chen, Yanlin Zhang, Srinidhi Varadharajan, Pierre Billon, Nikoleta Juretic, Craig Daniels, Amulya Nageswara Rao, Caterina Giannini, Eric M Thompson, Miklos Garami, Peter Hauser, Timea Pocza, Young Shin Ra, Byung-Kyu Cho, Seung-Ki Kim, Kyu-Chang Wang, Ji Yeoun Lee, Wieslawa Grajkowska, Marta Perek-Polnik, Sameer Agnihotri, Stephen Mack, Benjamin Ellezam, Alex Weil, Jeremy Rich, Guillaume Bourque, Jennifer A Chan, V Wee Yong, Mathieu Lupien, Jiannis Ragoussis, Claudia Kleinman, Jacek Majewski, Mathieu Blanchette, Nada Jabado, Michael D Taylor and Marco Gallo.
DOI: https://doi.org/10.1016/j.cell.2024.06.023
This work was supported by a Large-Scale Applied Research Project grant from Génome Quebec, Genome Canada, the Government of Canada and Ministère de l’Économie et de l’Innovation du Québec, with the support of the Ontario Research Fund through funding provided by the Government of Ontario. Further support was provided by Brain Canada Foundation through the Canada Brain Research Fund, Health Canada and the Azrieli Foundation through an Azrieli Future Leader in Canadian Brain Research grant, Canadian Institutes of Health Research (CIHR) project grants (PJT-156278 and PJT-173475), a CIHR postdoctoral fellowship and a Canada Research Chair.
About the RI-MUHC
The Research Institute of the McGill University Health Centre (RI-MUHC) is a world-renowned biomedical and healthcare research centre. The Institute, which is affiliated with the Faculty of Medicine of McGill University, is the research arm of the McGill University Health Centre (MUHC) – an academic health centre located in Montreal, Canada, that has a mandate to focus on complex care within its community. The RI-MUHC supports over 720 researchers and close to 1,400 research trainees devoted to a broad spectrum of fundamental, clinical and health outcomes research at the Glen and the Montreal General Hospital sites of the MUHC. Its research facilities offer a dynamic multidisciplinary environment that fosters collaboration and leverages discovery aimed at improving the health of individual patients across their lifespan. The RI-MUHC is supported in part by the Fonds de recherche du Québec – Santé (FRQS). www.rimuhc.ca
Media contact
Fabienne Landry
Communications coordinator, Research, MUHC
[email protected]
