SipSup nutrition program expands across MUHC
Nursing, nutrition, and pharmacy work together to help improve the nutritional status of patients.
“Did you know that 45 percent of patients admitted to Internal Medicine at the Montreal General Hospital (MGH), and 42% at the Royal Victoria Hospital (RVH) are at risk of being malnourished or suffer from malnutrition?”
I thought I had heard wrong. What, almost half of admitted patients? I stayed silent, staring at my notes.
Deborah Fleming, MUHC manager of Clinical Nutrition (adult sites), translated my thoughts: “I know, it’s surprising. And this happens in all hospitals across the country. It is a very serious issue.”
Serious enough for Deborah and her colleague Ann Coughlin, assistant manager of Clinical Nutrition (adult sites), to implement a program to help improve the nutritional status of patients that firstly started in the Department of Internal Medicine of the MGH in 2016, and now expanding it across MUHC.

With the SipSup program, a small volume of a nutritionally dense supplement is given by nurses to malnourished or at risk patients twice a day, at the same time as medication is administered. Supplements are served in a small portion (half a cup or 115 mL) so patients still have enough appetite to eat their food. They can be served as either a liquid, for patients who can eat regular textures, or as a pudding, for patients who have difficulty swallowing. Each portion gives patients an extra 9 grams of protein and 220 calories, to help towards repairing, building and maintaining cells and body tissues.
“We know that patients are more likely to drink supplements when they are given directly by a nurse at the same time the medication is given, says Deborah Fleming.
A new screening tool
This year, the team at the adult sites has introduced a tool to better screen patients at the time of admission. “We will be implementing a validated screening questionnaire to be used by nutrition technicians to collect the information from patients, explains Deborah, with two short questions:
- Have you lost weight in the last six months (without trying)?
- Have you been eating less than usual for more than a week?”
“Two ‘yes’ answers indicate a nutrition risk,” says Ann, and our mission is to put our efforts to lower this risk. Screening allows us to flag patients who would benefit from SipSup as soon as possible.”
The Lachine Hospital has been using this questionnaire to screen patients since 2015. “We were providing supplements on the meal tray to patients who were screened at risk” explains Pina Ventulieri, Manager, Multidisciplinary Services at the Lachine Hospital. “As of October, we will harmonize our program with the rest of the MUHC and provide the supplements by a nurse at the same time as the medication.”
Overcoming barriers: new challenges
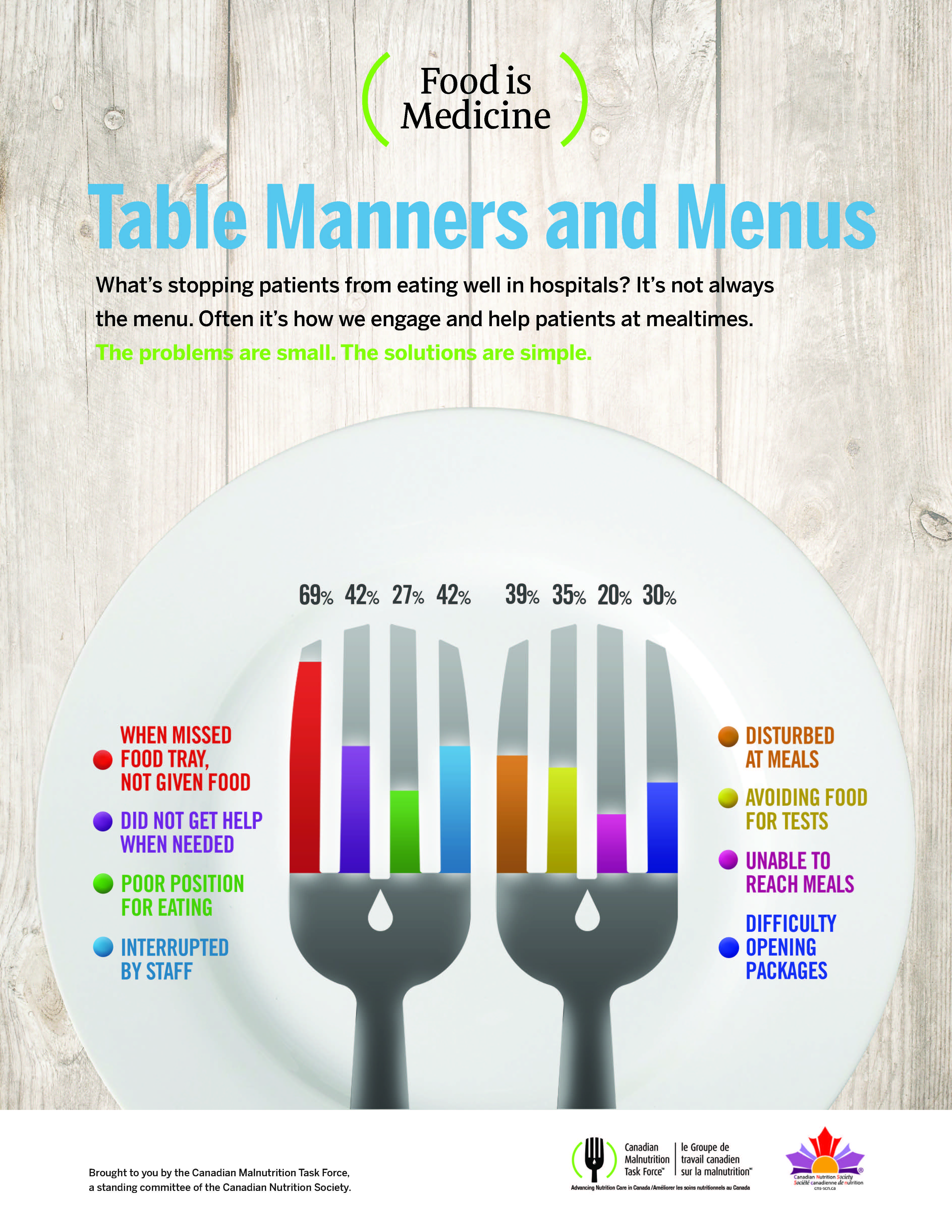
It is widely recognized that the hospital environment can often present barriers to patients’ ability to meet nutrition goals, as shown in this diagram:
Confronted with any of these barriers, a patient who is admitted already at risk or with malnutrition can face serious nutrition consequences.
The SipSup program offers a first line measure to both overcome nutrition risk and offset some of these potential barriers.
Its success relies on a team approach where nursing, nutrition, and pharmacy work together to make a difference while the patient is in hospital.
“Discharged patients are still in a phase of recovery and need to continue to eat well to heal,” says Deborah. “Since malnourished patients are at higher risk of readmission, it is important to reduce these rates with early detection and intervention.”
Nutritional risk among older Canadians
- 34% of Canadians aged 65 or older are at nutritional risk
- Women are more likely than men to be at risk.
- Among people with depression, 62% were at nutritional risk, compared with 33% of people without depression.
- Disability, poor oral health, and medication use are associated with nutritional risk, as are living alone, low social support, infrequent social participation, and not driving on a regular basis.
- Lower income and education were also associated with nutritional risk.
Source: Nutritional risk among older Canadians, (Research article) by Pamela L. Ramage-Morin and Didier Garriguet